AbstractPurposeThis study aimed to examine the health concerns of parents regarding their premature infants and to identify changes in these concerns during perinatal period and after discharge.
MethodsThis was a retrospective study performed at a single tertiary center that enrolled 119 premature infants who were discharged from the neonatal intensive care unit (NICU) and visited the outpatient pediatrics department between December 2018 and October 2021. Data on the concerns of 176 parents regarding enrolled premature infants’ health from before birth to 1 week after NICU discharge were obtained from outpatient records. The t test and with the chi-squared test were used to analyze the data for this study.
ResultsThe consistently greatest focus of parents' health concerns was the respiratory system. The second focus of parents' health concerns before discharge was the central nervous system. However, during the first week after NICU discharge, the gastrointestinal system was the second-most frequent focus of parents’ health concerns among parents of infants without diseases related to prematurity and infants with older gestational ages.
ConclusionThe results of this study offer insights into the health concerns among parents of premature infants. Parental health concerns about premature infants vary over time, from before birth to post-discharge, necessitating supportive interventions to enhance parental understanding of their child's health status.
INTRODUCTIONPreterm birth rates are increasing worldwide [1]. In addition, according to the Korea National Statistical Office, the proportion of premature births in Korea increases every year. In 2021, the proportion of premature births (<37 weeks of gestation) was 9.2%, which was a 0.7% increase from that of the previous year [2]. Correspondingly, the prevalence of prematurity-related diseases is also increasing [3]. Prematurity is the main cause of neonatal death globally. Preterm birth consequences lead to a higher risk of neurological, cognitive, sensory, respiratory, digestive, renal, cardiovascular, metabolic, immune, and psychosocial disturbances in both the short and long term. Pathologies related to prematurity include respiratory distress disease (RDS), necrotizing enterocolitis (NEC), retinopathy of prematurity (ROP), and intraventricular hemorrhage (IVH) [4,5]. Preterm infants have a higher risk of developing bronchopulmonary dysplasia (BPD), pulmonary hypertension, asthma, cerebral palsy, cognitive disability, and seizure disorders as long-term consequences [4].
Furthermore, data regarding various diseases that are related to premature birth can easily be accessed on the Internet, and medical data about which diseases occur most frequently after birth are well-documented [6]. The risks for preterm infants do not end after hospitalization, and they continue to have high vulnerability even after discharge. The care they receive at home has a crucial impact on their well-being in the long term [7].
Therefore, parents of premature infants can have negative thoughts and fears [8,9], and numerous articles about their emotional stress have been published. In addition, many studies have been published about parental stress caused by the medical conditions of their infants, the prematurity of their infants [10-12], and a lack of information about the diagnosis or treatment of their infants [12]. Therefore, many studies have been conducted on the emotional experiences of the parents of infants hospitalized in the neonatal intensive care unit (NICU). Their highest stressor was the parental role, and parental stress was influenced by the length of the NICU stay, gestational age, infant's need for respiratory support, and cardiovascular diagnosis [8,10]. Parents experienced difficulties in coping with hospitalization stress, grief, isolation, and a lack of preparation for the transition to parenthood [13]. Therefore, it is necessary to identify parental risk factors immediately after preterm birth to assist in reducing parents' negative emotions and stress [8], and parents need to be prepared for the transition of childcare from the hospital to home. The process of preparing parents for preterm infant care should be gradual and dynamic, starting from admission. Through this preparation, parents acquire the knowledge and skills needed to care for preterm infants at home, as well as emotional stability and a sense of security. The preparation process for transitioning from the NICU to home should be tailored to the individual social circumstances of the parents, and the specific conditions and needs of each preterm infant. The child’s clinical progression and the parents' adaptation to the situation should also be considered [14]. Parents of preterm infants in Korea have supportive care needs, including a vague fear of caring for a baby upon imminent NICU discharge, real-world difficulties encountered while caring for preterm children, concerns about growth and development problems, and anxiety about possible complications [15].
However, there has been little research on the health problems of the greatest parental concern in their premature infants and whether these concerns change over time in South Korea. The purpose of this study was to identify health-related concerns among the parents of preterm infants, changes in their parental concerns over time, and the factors that affected them during the perinatal period and after discharge. In addition, based on the results of this study, basic data for developing supportive care interventions according to parents’ concerns that change from the birth of a premature baby to after discharge from the hospital was provided.
METHODSEthics statement: This study was approved by the Institutional Review Board (IRB) of Kosin University Gospel Hospital (No. 2022-03-045). This study received a consent waiver.
1. Study DesignThis was a retrospective study [16] in which data were obtained and analyzed through the contents of outpatient medical records for premature infants. This retrospective study investigated the concerns of the mothers and fathers of premature infants through medical examinations during outpatient visits. The reporting of this study was based on the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guidelines [17].
2. Study Setting and ParticipantsThe researchers intended to record the medical aspects of parents’ concerns about their infants in order to help support parenting interventions while performing long-term follow-up management of preterm infants when they return to the hospital for their first outpatient visit after discharge from the NICU. As established by a previous study [18], the researchers interviewed parents of premature infants in the outpatient department (OPD) about concerns regarding neonatal problems related to preterm birth and let them select one answer (Supplement 1. Questionnaire). Data obtained longitudinally were analyzed to extract data cross sectionally.
In this study, 177 premature infants who visited the neonatal clinic of the Department of Pediatrics between December 1, 2018, and October 31, 2021, were investigated. These infants with <37 weeks of gestation were born at the hospital, hospitalized, and discharged from the NICU. The hospital is a level III unit with 18 NICU beds. Information about parents’ health concerns regarding their premature infants was recorded in the OPD chart. Parents who were not asked for information about their concerns regarding the health of their preterm infants (n=39), preterm infants who were transferred from other hospitals (n=17), and infants who died (n=2) were excluded from this study. No infants with congenital anomalies were enrolled. Finally, 119 premature infants were included in this study, and information was gathered from a total of 176 parents, as 57 out of the 119 premature infants had both the father and mother responding.
3. Variables1) Clinical characteristics of premature infantsThe clinical characteristics of premature infants included gestational age, birth weight, sex, delivery type, 1- and 5-minute Apgar scores, the first baby or not, total length of hospital stay, need for resuscitation and blood transfusion, disease, and central catheter insertion.
2) Maternal characteristicsThe maternal characteristics included maternal age and maternal pregnancy complications (e.g., pregnancy-induced hypertension, gestational diabetes mellitus, hyperthyroidism, and hypothyroidism) were investigated.
3) Parents’ greatest concerns regarding their premature infants’ healthThe questionnaire in this study consisted of 1 item to investigate either the father or mother and 5 items regarding the greatest concerns with their infants’ health at five different times: before birth, immediately after birth, 7 days after birth, before hospital discharge, and 1 week after hospital discharge to home (Supplement 1. Questionnaire).
4. Data CollectionThis study was conducted after receiving approval for the research plan and a waiver of informed consent from the institutional review board (IRB) of the university hospital. The electronic medical records (EMRs) of the patients were collected as anonymous data with the cooperation of the medical information management office from December 1, 2018, to October 31, 2021. Neonatal problems associated with premature birth are classified in pediatric textbooks by organ system as follows: respiratory, cardiovascular, hematologic, gastrointestinal (GI), metabolic endocrine, central nervous system (CNS), renal, and infection [6]. Common problems in premature infants arise in these systems and are explained to the parents on the day of neonatal admission to the NICU. Both during hospitalization and upon discharge from the NICU, parents were provided with documents summarizing the medical conditions of their infants and any consequences that occurred during hospitalization. During outpatient visits, diseases of prematurity that had been explained during hospitalization and upon discharge were fully explained again, and the parents' concerns about their infants’ health were confirmed in the outpatient clinic during follow-up and management of the premature infants. Based on a previous study during which Korean mothers of premature infants were interviewed regarding emotional adjustment and concerns at five distinct points in time from immediately after NICU hospitalization to infant discharge [9], parents were also asked about their greatest health concerns regarding their infants at different times, including before birth, immediately after birth, 7 days after birth, before hospital discharge, and 1 week after hospital discharge to home [18], and their answers were recorded on the outpatient medical records forms. We investigated these data in this study because parental responses and stress are influenced by obstetric and infant characteristics [19].
5. Data AnalysisThe investigated items were entered into Microsoft Excel (Microsoft Corp.) for management and IBM SPSS Statistics version 25.0 (IBM Corp.) for the comparison of continuous variables with the t test and of categorical variables with the chi-squared test [20]. All test results with p<.05 were considered statistically significant.
RESULTS1. Clinical Characteristics of Premature Infant and Maternal Characteristics of Their Mothers
Table 1 shows the infant, obstetric, and parental characteristics. The mean gestational age of the infants was 33.02±2.91 weeks (23.86–36.86 weeks). The mean birth weight was 1,991.53±570.84 g (600.00–3,600.00 g). There were 69 males (58.0%) and 50 females (42.0%). The mean Apgar scores at 1 and 5 minutes were 6.37±1.63 (1–9 range) and 8.15±1.01 (5–9 range), respectively. Most parents had no other children (67/119 cases [56.3%]), and most infants were born via cesarean delivery (84.0%). The number of infants who needed resuscitation at birth, blood transfusions, and central catheter insertion were 14 (11.8%), 17 (14.3%), and 61 (51.3%), respectively. The mean total length of the infants’ hospital stay was 40.64±31.74 days (8–166 days). Among the infants, 37 (31.1%) were diagnosed with RDS, 25 (21.0%) with BPD, 25 (21.0%) with patent ductus arteriosus, 4 (3.4%) with ROP, 19 (16.0%) with IVH, 6 (5.0%) with periventricular leukomalacia (PVL), and 22 (18.5%) with sepsis. There were some infants who had multiple overlapping diseases. The mean age of the mothers was 33.34±4.84 years (22–44 years) and maternal pregnancy complications occurred in 42 infants (35.3%) (Table 1). Among the responders, 113 were mothers (64.2%) and 63 were fathers (35.8%), with no statistically significant difference in responder type.
2. Parental Concerns about Prematurity-related DiseasesThe analysis of parents’ concerns about their premature infants revealed that most parents were concerned about their respiratory system throughout the entire period from before birth to 1 week after NICU discharge (Figure 1). Throughout the entire period, it can be seen in Figure 1 that parents showed the most concern about the respiratory system after birth, with responses from 77 mothers (77/123, 62.6%) and 46 fathers (46/123, 37.4%). In addition, the CNS was the second most concerning system from before birth until before discharge and statistically significant differences were observed before and after birth. Furthermore, during the first week after hospital discharge, the second most concerning system shifted to the GI system from the CNS, and the degree of concern regarding the GI system during the first week after hospital discharge significantly increased when compared to respectively different points in time, such as before birth, after birth, seven days after birth, and before discharge (Figure 1).
3. Differences in Infants and Maternal Characteristics Between the Greatest and Second-greatest Concerns of Parents
Table 2 presents the data and results for the greatest and second-greatest concerns of parents about their premature infants according to time. The premature infants of parents with respiratory system concerns after birth had younger gestational ages; moreover, a substantial percentage of these infants had a birth weight of <1,500 g (Table 2). Respiratory system concerns significantly increased after birth compared to those before birth (98 vs. 123 respondents, respectively; p<.001) (Figure 1). The only related factor that was associated with respiratory system concerns pre-birth was cesarean delivery; however, cesarean delivery was a statistically significant factor associated with respiratory system concerns during the entire study period (Table 2). The average 1- and 5-minute Apgar scores of the infants of parents with respiratory system concerns were also considerably lower than those of infants whose parents had different concerns (Table 2). The parents of infants with a diagnosis of RDS and the parents of infants with a diagnosis of BPD before discharge had significant concerns about the respiratory system. Moreover, parental concerns about the respiratory system were significantly affected by transfusion requirements after birth, longer phototherapy within 7 days after birth, longer antibiotic treatment during the hospital stay before discharge, and longer hospital duration (Table 2).
Concerns about the CNS system were the second-most common type from before birth to before hospital discharge. Concerns about the CNS decreased after birth compared to those reported before birth (25 vs. 15 respondents, respectively; p<.001) (Figure 1). However, concerns about the CNS subsequently increased again to a level similar to that seen immediately before birth and before hospital discharge (Figure 1). Most of the parents of infants with a diagnosis of IVH or PVL before discharge also had significant CNS concerns (Table 2). Parents of infants with a gestational age of less than 32 weeks had the second-greatest concerns about the CNS before birth and at seven days after birth.
Table 3 shows that concern about the GI system was the second-most common at 1 week after discharge from the NICU and was compared to other organ systems. These concerns significantly increased after discharge compared to those before birth, after birth, 7 days after birth, and before discharge (37 vs. 10, 13, 22, and 21 respondents; p<.05) (Figure 1). As a result of analyzing the factors that increased concerns about GI problems during the post-hospital period, the gestational ages of the infants of parents with GI concerns (33.90±2.48 weeks) were significantly increased compared to those of the infants of parents who had other concerns (32.78±2.98 weeks; p=.039) (Table 3). Other significant factors included birth weights of ≥1,500 g (p=.021) and the absence of diagnoses of RDS (p=.030), ROP (p=.014), or IVH (p=.007) (Table 3). The duration of antibiotic treatment for infants whose parents had concerns about their GI systems was shorter than that of infants whose parents had concerns about other organ systems.
DISCUSSIONThe parents of premature infants in this study were the most concerned about the respiratory system at all times from before birth to 1 week after NICU discharge to home, which was similar to the results of a previous study [18]. This concern was probably the greatest because proper breathing is the most crucial aspect for life after birth [21]. Moreover, no differences in responses existed between mothers and fathers in this study. Unlike the differences found between mothers and fathers in terms of emotional stress experienced by the parents of premature infants [7,15], it was evident that mothers and fathers shared the same medical health concerns during the current study. The existence of this similarity is plausible because it is generally well-known that proper breathing is the most important aspect of life after the birth of a premature infant [22]. Although cesarean delivery was one of the risk factors for respiratory system concerns throughout the study period, it was the only statistically significant risk factor for the existence of concerns regarding the respiratory system during the prepartum period. It is a commonly accepted fact that, compared with vaginal delivery, cesarean delivery is associated with greater risks for diseases related to respiration in newborns [23]. Furthermore, this is also due to the fact that cesarean delivery is the only factor among those considered that the general public can easily explore and understand through websites, books, or television programs that provide information about pregnancy and childbirth. Respiratory system concerns were also more common after birth among parents whose premature infants had birth weights <1,500 g or younger gestational ages. There was a significant increase in concerns compared to those present before birth because newborns with younger gestational ages at birth or lower birth weights are more likely to experience respiratory problems. In addition, there were clearly other common characteristics of preterm infants whose parents were concerned about respiratory problems, including lower 1- and 5-minute Apgar scores, a diagnosis of RDS, a diagnosis of BPD, and the need for blood transfusions. This result suggested that parents of premature infants with low gestational age or low birth weight were concerned about the respiratory system because their infants had experienced RDS immediately after birth, or had sometimes been diagnosed with BPD.
In this study, the second-most common concern was CNS disorders from before birth to before hospital discharge. In previous studies [18], the second-most common parental concerns were focused on the CNS, cardiovascular system, GI system, and infection, and these varied according to time (with no significant differences among times). In the present study, the mean gestational age and mean birth weight were lower (33.0±2.9 weeks and 1,991.5±570.8 g) than the values reported by previous investigators (33.1±3.0 weeks and 2,124.4±685.1 g) [13]. Overall, the premature infants of parents who had CNS concerns had the lowest gestational ages; however, this trend was not statistically significant, and it was not affected by birth weight. Only the parents of premature infants diagnosed with brain abnormalities, such as IVH or PVL had statistically significant increases in CNS concerns. This result could be due to the bias caused by intervention by the medical staff because parental interviews were conducted due to the presence of brain abnormalities. However, this could also have occurred because the mothers were focused on the current conditions and future development of their infants [9,24], and because concerns about CNS disorders are naturally common among parents of premature infants. In addition, mothers who are aware of serious problems in their premature infants continue to experience guilt and worry about the health of their infants [9]. Concerns about CNS development are inevitable because of the long-term consequences.
When the gestational age was older and the infants had no disease specifically attributable to prematurity, concerns about the GI system were the second-most common health concerns among parents at 1 week after NICU discharge. This trend might have existed because changes in the health concerns of parents were similar to the changes in their emotions after hospital discharge [9,25,26]. When infants are in objectively good health, parents feed them directly and witness their development at home after discharge, unlike in the hospital. It was also evident that GI system concerns among parents increased as infants spent more of their time consuming formula or breast milk and sleeping; these are activities that parents directly engage in to support their fragile infants so that they can grow in good health at home. Therefore, parents had high levels of concern about the GI system related to feeding, in which the rate of parental involvement is high, even when their premature babies did not have any specific GI disease and had an older gestational age. It has been said that most of the reasons why late preterm infants are often readmitted within the first 7 to 10 days after discharge are problems related to feeding [27,28]. This could result in increased GI concerns during the post-discharge period. Under these circumstances, parents are mainly interested in factors related to infant nutritional status and follow-up care, with the expectation that their premature infants will develop normally after discharge [9].
Therefore, health care providers will be able to proactively provide psychological support, education, and intervention by offering GI-specific information and support during outpatient care of preterm infants, knowing that parents have concerns about the GI system after discharge. In addition, it would be valuable to conduct a clinical study to confirm the results of intervention when educational support regarding the development of the digestive system in premature infants and the prevention of digestive issues is prospectively provided to parents during neonatal transitional care in discharge education given the retrospective evaluation results of this study. After the most common type of concerns (regarding the respiratory system) was excluded, the next-most common concern varied for parents of premature infants at the time of discharge from the NICU. This result was significantly dependent on the gestational age at birth and the specific diseases diagnosed. This could be the result of the emotional changes that occur in mothers as their focus shifts from survival to caring for their physically frail infants at home after discharge [9]. Knowledge that the focus of the parents of premature infants changes over time, especially after NICU discharge, may be helpful when supporting parents with concerns after discharge and may improve outpatient follow-up care of premature infants. The long-term relief of parents’ emotional and medical concerns might be achieved through additional research and analysis of changes in parents’ concerns and identifying factors that affect these changes at milestones during the development of their premature infants.
In conclusion, proactive strategies are necessary to promote the growth and development of preterm infants and to meet parental healthcare needs for premature infants after NICU discharge. The level of preparation for the transition to home of a premature baby can impact parent and child survival and fitness. Healthcare professionals must provide education on respiratory and GI care during the transitional period during hospitalization before discharge because the growth and development trajectory of premature babies can be markedly different from those of a term infant and tailored support may be needed [29]. It is necessary to offer tailored education to parents based on the specific characteristics of their preterm infant, considering factors including gestational age, birth weight, and CNS conditions. However, research on the supportive care needs and interventions for parents of preterm infants is insufficient in South Korea [15]. Therefore, we suggest the longitudinal assessment of specific needs based on the concerns of parents of premature infants from before birth to post-discharge, and the development and implementation of supportive interventions to meet those needs during each phase.
This study had several limitations. First, because this study only included participants from a single NICU and of a single ethnic group and because the distributions of gestational age and birth weight were not even among study participants, the study findings are not representative of the entire population. Second, memory bias might have influenced the results because parents of premature infants were asked to recall information about their health concerns. Finally, the number of participants was small; therefore, further large-scale studies are necessary.
CONCLUSIONAmong parents of premature infants, the most common focus of medical concerns in the period from birth to 1 week after NICU discharge was the respiratory system. The second-most common focus of medical concerns after NICU discharge changed based on the gestational age and diseases of the premature infants. This information may help to increase the understanding of the health concerns of parents about their infants from before birth to after NICU discharge and how these concerns may change over time. Therefore, it is necessary to develop and implement supportive interventions to reduce parental anxiety when caring for their premature infants. In addition, it is essential to offer multidisciplinary interventions involving doctors, nurses, development experts, and others, to support the individual growth and development of preterm infants and to assist in managing complications.
NotesAuthors' contribution
Conceptualization: all authors; Data collection, Formal analysis: all authors; Writing-original draft: all authors; Writing-review and editing: all authors; Final approval of published version: all authors.
Conflict of interest
No existing or potential conflict of interest relevant to this article was reported.
REFERENCES1. Walani SR. Global burden of preterm birth. International Journal of Gynaecology and Obstetrics. 2020;150(1):31-33. https://doi.org/10.1002/ijgo.13195
2. Statistics Korea. Birth statistics in 2021 [Internet]. 2021 [cited 2022 August 28]. Available from: https://kostat.go.kr/board.es?mid=a10301020300&bid=204
3. Behrman RE, Butler AS. Preterm birth: causes, consequences, and prevention. National Academies Press; 2007. p. 31-52.
4. Pravia CI, Benny M. Long-term consequences of prematurity. Cleveland Clinic Journal of Medicine. 2020;87(12):759-767. https://doi.org/10.3949/ccjm.87a.19108
5. Pinto F, Fernandes E, Virella D, Abrantes A, Neto MT. Born preterm: a public health issue. Portuguese Journal of Public Health. 2019;37(1):38-49. https://doi.org/10.1159/000497249
6. Brady JM, Barnes-Davis ME, Poindexter BB. The high-risk infant. In: Kliegman RM, St. Geme JW 3rd, Editors. Nelson textbook of pediatrics. 21st ed. Elsevier; 2020. p.897-909.
7. Gardon L, Picciolini O, Squarza C, Frigerio A, Giannì ML, Gangi S, et al. Neurodevelopmental outcome and adaptive behaviour in extremely low birth weight infants at 2 years of corrected age. Early Human Development. 2019;128:81-85. https://doi.org/10.1016/j.earlhumdev.2018.12.013
8. Ionio C, Mascheroni E, Colombo C, Castoldi F, Lista G. Stress and feelings in mothers and fathers in NICU: identifying risk factors for early interventions. Primary Health Care Research & Development. 2019;20:e81. https://doi.org/10.1017/s1463423619000021
9. Lee IH, Norr KF, Oh K. Emotional adjustment and concerns of Korean mothers of premature infants. International Journal of Nursing Studies. 2005;42(1):21-29. https://doi.org/10.1016/j.ijnurstu.2004.05.004
10. Dudek-Shriber L. Parent stress in the neonatal intensive care unit and the influence of parent and infant characteristics. American Journal of Occupational Therapy. 2004;58(5):509-520. https://doi.org/10.5014/ajot.58.5.509
11. Franck LS, Cox S, Allen A, Winter I. Measuring neonatal intensive care unit-related parental stress. Journal of Advanced Nursing. 2005;49(6):608-615. https://doi.org/10.1111/j.1365-2648.2004.03336.x
12. Sikorova L, Kucova J. The needs of mothers to newborns hospitalised in intensive care units. Biomedical Papers of the Medical Faculty of the University Palacky, Olomouc, Czechoslovakia. 2012;156(4):330-336. https://doi.org/10.5507/bp.2011.046
13. Whittingham K, Boyd RN, Sanders MR, Colditz P. Parenting and prematurity: understanding parent experience and preferences for support. Journal of Child and Family Studies. 2014;23(6):1050-1061. https://doi.org/10.1007/s10826-013-9762-x
14. Osorio Galeano SP, Salazar Maya ÁM. Preparing parents for discharge from the neonatal unit, the transition, and care of their preterm children at home. Investigacion y Educacion en Enfermeria. 2023;41(1):e04. https://doi.org/10.17533/udea.iee.v41n1e04
15. Park JH, Lee H, Cho H. Analysis of the supportive care needs of the parents of preterm children in South Korea using big data text-mining: topic modeling. Child Health Nursing Research. 2021;27(1):34-42. https://doi.org/10.4094/chnr.2021.27.1.34
16. Kim DJ, Kil SY, Son J, Lee HS. How to conduct well-designed clinical research. Kosin Medical Journal. 2022;37(3):187-191. https://doi.org/10.7180/kmj.22.122
17. von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP; STROBE Initiative. Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. British Medical Journal. 2007;335(7624):806-808. https://doi.org/10.1136/bmj.39335.541782.ad
18. Lee JY, Lee JH, Yeon GM, Jung YJ. Parental anxiety regarding premature infants and factors affecting parental concern. Journal for Specialists in Pediatric Nursing. 2019;24(4):e12266. https://doi.org/10.1111/jspn.12266
19. Baía I, Amorim M, Silva S, Kelly-Irving M, de Freitas C, Alves E. Parenting very preterm infants and stress in neonatal intensive care units. Early Human Development. 2016;101:3-9. https://doi.org/10.1016/j.earlhumdev.2016.04.001
20. Kang G, Kim SE. How to write an original article in medicine and medical science. Kosin Medical Journal. 2022;37(2):96-101. https://doi.org/10.7180/kmj.22.105
21. van Vonderen JJ, Roest AA, Siew ML, Walther FJ, Hooper SB, te Pas AB. Measuring physiological changes during the transition to life after birth. Neonatology. 2014;105(3):230-242. https://doi.org/10.1159/000356704
22. Helin I. Mother-infant relationships in the NICU: a multiple case study approach [dissertation]. Chicago: Loyola University; 2015. p. 1-280.
23. Tefera M, Assefa N, Mengistie B, Abrham A, Teji K, Worku T. Elective cesarean section on term pregnancies has a high risk for neonatal respiratory morbidity in developed countries: a systematic review and meta-analysis. Frontiers in Pediatrics. 2020;8:286. https://doi.org/10.3389/fped.2020.00286
24. Srivastav D, Lal Mathur MN. Helicopter parenting and adolescent development: from the perspective of mental health. In: Benedetto L, Ingrassia M, Editors. Parenting - studies by an ecocultural and transactional perspective. IntechOpen; 2020. p. 71-90.
25. Holditch-Davis D, Santos H, Levy J, White-Traut R, O'Shea TM, Geraldo V, et al. Patterns of psychological distress in mothers of preterm infants. Infant Behavior & Development. 2015;41:154-163. https://doi.org/10.1016/j.infbeh.2015.10.004
26. Leahy-Warren P, Coleman C, Bradley R, Mulcahy H. The experiences of mothers with preterm infants within the first-year post discharge from NICU: social support, attachment and level of depressive symptoms. BMC Pregnancy and Childbirth. 2020;20(1):260. https://doi.org/10.1186/s12884-020-02956-2
27. Young PC, Korgenski K, Buchi KF. Early readmission of newborns in a large health care system. Pediatrics. 2013;131(5):e1538-e1544. https://doi.org/10.1542/peds.2012-2634
28. Ray KN, Lorch SA. Hospitalization of early preterm, late preterm, and term infants during the first year of life by gestational age. Hospital Pediatrics. 2013;3(3):194-203. https://doi.org/10.1542/hpeds.2012-0063
29. Green J, Fowler C, Petty J, Whiting L. The transition home of extremely premature babies: an integrative review. Journal of Neonatal Nursing. 2021;27(1):26-32. https://doi.org/10.1016/j.jnn.2020.09.011
Figure 1.Parents’ health concerns about the health problems of their premature infants according to time (*p<.05). 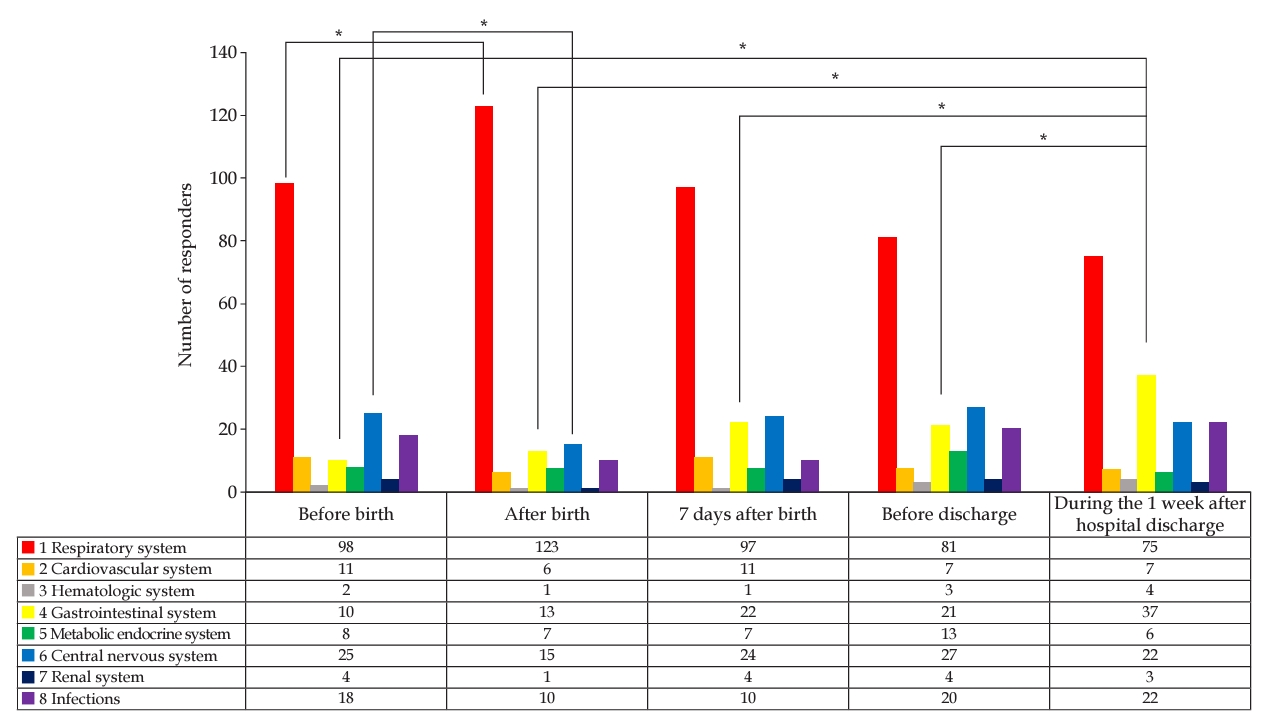
Table 1.Patient Characteristics of the Premature Infants (N=119) and Their Parents (N=176) Table 2.Parental First and Second Health Concerns Regarding Preterm Infants According to Time (N=176) a)p<.05; BPD, bronchopulmonary dysplasia; CNS, central nervous system; Cx., complications; GI, gastrointestinal; IVH, intraventricular hemorrhage; M, mean; PDA, patent ductus arteriosus; PVL, periventricular leukomalacia; RDS, respiratory distress syndrome; Resp., respiratory; ROP, retinopathy of prematurity; SD, standard deviation; TPN, total parenteral nutrition; Tx., treatment. Table 3.Concerns of Parents about the GI System Compared to Those about Other Organ Systems at 1 Week after Hospital Discharge (N=176) |
| |||||||||||||||||||||||||||||||||||||||