Family resilience and caregiver’s well-being across different age groups of children with ADHD in the United States: a cross-sectional study
Article information
Abstract
Purpose
This study aimed to investigate the impact of family resilience on caregiver well-being across various age groups of children diagnosed with ADHD (attention-deficit/hyperactivity disorder) groups (0–5, 6–11, and 12–17 years).
Methods
Utilizing secondary data from the 2022 US National Survey of Child Health, this cross-sectional study involved 2,752 children who were formally diagnosed with ADHD. Statistical analysis included descriptive analysis, Spearman’s rank correlation, chi-square tests, and linear regression, conducted using SPSS version 27.
Results
The study revealed a moderate positive correlation (r=.35, p<.001) between family resilience and caregiver well-being. Controlling for covariates, family resilience accounted for 25.2%, 21.1%, and 22.1% of caregiver well-being variance in age groups 0–5, 6–11, and 12–17 years, respectively. Additionally, factors like employment status, family structure, and caregiver age showed varying influences on caregiver well-being across these developmental stages. A consistent pattern emerged across these age groups: unemployment and non-traditional family structures were associated with negative impacts on caregiver well-being, whereas older caregiver age positively influenced well-being.
Conclusion
This research underscores the importance of age-specific family resilience strategies to improve caregiver well-being and family interactions in ADHD contexts. Investigating these aspects through qualitative studies across various cultures could deepen our understanding of well-being and inform culturally sensitive interventions.
INTRODUCTION
Attention-deficit/hyperactivity disorder (ADHD), characterized by symptoms such as impulsivity, hyperactivity, and difficulties in sustaining attention [1], is estimated to impact around 7.2% of the global population. The early indicators of hyperactivity in ADHD are typically not easily noticeable until a child reaches around four years old, becoming more apparent during their elementary school years. The condition’s progression usually follows a recognizable trajectory into early adolescence [2]. In preschool-aged children with ADHD, common symptoms include poor concentration, high levels of activity, impulsiveness, alongside developmental delays, oppositional behavior, and poor social skills. As these children reach school age, they often encounter academic failure, peer rejection, and low self-esteem, which specific learning difficulties in some cases can further complicate. Moving into adolescence, the overt hyperactivity typically seen in younger children with ADHD tends to decrease, but challenges such as inattention, impulsiveness, and internal restlessness persist. Adolescents with ADHD may also struggle with a distorted sense of self and disruptions in their self-identity development, coupled with an increased likelihood of exhibiting aggressive and antisocial behaviors [3]. The American Association of Pediatrics guidelines categorize ADHD management by age groups: 4–5 years, 6–11 years, and 12–18 years, focusing primarily on behavioral therapy [4]. In young children, the therapeutic approach centers on training parents in management techniques, while for older children, therapy integrates family-oriented strategies to enhance organizational and impulse control skills, nurturing the child’s self-regulation and organizational capabilities.
Caring for children with ADHD can be challenging for caregivers, often leading to frustration due to the complexities in managing the children’s behavioral issues, disruptions in social and family dynamics, emotional and physical fatigue, as well as financial burdens [5]. If caregivers’ concerns and requirements are not properly acknowledged and if there is a lack of tailored interventions to alleviate their caregiving difficulties, it could lead to a compromise in their mental and physical health [5]. Consequently, this situation might also hinder the caregivers’ ability to provide the necessary and appropriate care to the children. When well-being is ignored, children may be impacted. Caregivers experiencing depression can significantly impact the symptomatology of ADHD in children [6]. Well-being, defined as a subjective perception and assessment of one’s life and self, characterized by subjective experiences and feelings [7], is crucial for caregivers. Improved caregiver well-being is linked to better mental and physical health and is associated with a lower risk of mortality [8]. When caregivers maintain good mental health, they are better equipped to engage in and foster resilience-building behaviors within the family [9].
Family resilience is characterized by the capability to endure and bounce back from challenges, becoming stronger and more resourceful in the process [10], and is particularly relevant in families with children who have chronic illnesses like ADHD [11]. It involves systemic and relational processes in families, including belief systems, organizational patterns, and communication/problem-solving processes. This can be measured by how the family recognize strength, maintains hope, communicates, and works to solve the problem [12]. The improvement of family resilience not only strengthens family cohesion but also enhances overall family well-being [13]. Further, family cohesion acts as a protective factor which diminishes the relationship between subjective and objective burdens, considered as well-being, perceived by caregivers [14]. This is especially pertinent as different age groups of children with ADHD interact with family resilience and caregiver well-being in varied ways. At the time of diagnosis, family resilience is indispensable. This need becomes even more pronounced in families with adolescents, who face significant adversities, including societal stigma [13] and an increased risk of depression among adolescents [15]. However, in the realm of ADHD research, the majority of studies on family resilience have focused on its effects on children [15-17], with limited attention given to caregivers. Therefore, this study will expand knowledge about how to improve the well-being of caregivers of children with ADHD.
This research aims to investigate the impact of family resilience on caregiver well-being across various age groups of children diagnosed with ADHD groups (0–5, 6–11, and 12–17 years) and to explore how different covariates such as employment status, family structure, and caregiver’s age influence this relationship. We hypothesize that higher levels of family resilience are positively associated with caregiver’s well-being across different age groups of children with ADHD (H1), family resilience impacts differently on caregiver’s well-being across different child age groups (H2), and specific covariates (child’s sex, language, caregiver’s sex, age, employment status, family structure, and race) have distinct impacts on caregiver well-being in each age group (H3). Variations in well-being across different age groups present a significant concern in the field of mental health and wellness. Understanding the role of family resilience in these variations is crucial for developing age-specific interventions and support systems.
METHODS
Ethics statement: As the study used secondary data which does not contain respondent’s identity, IRB is not required. The author received permission from the National Survey of Children Health to use part of the data for this study.
1. Study Design and Data Collection
This research utilized a cross-sectional design, analyzing secondary data collected from July 2022 to January 2023. The analysis itself was conducted over a subsequent period, from July to December 2023. The data were derived from the 2022 US National Survey of Children’s Health (NSCH) [18]. This annual survey is carried out to gather data on the physical and emotional well-being of children aged 0 to 17 years across the US [18]. The dataset, publicly accessible, was obtained in SAS format. For this research, the authors received explicit authorization from the US Census Bureau to utilize the data. Rigorous data cleaning procedures were implemented, resulting in a final sample of 2,752 children aged 0 to 17 years diagnosed with ADHD. The primary caregivers of these children served as the respondents for this study. Adherence to the STROBE (Strengthening the Reporting of Observational Studies in Epidemiology) guidelines ensures that the manuscript can be thoroughly understood and rigorously evaluated by the reader [19].
2. Participants
Inclusion criteria for the children in this study were based on a positive response to the question regarding current symptoms of ADHD/ADD (attention deficit disorder), following a formal diagnosis. The children with ADHD were stratified into three age groups for analysis: T1 (0–5 years), T2 (6–11 years), and T3 (12–17 years). The respondents, encompassing primary caregivers, were representative of a diverse demographic, hailing from various states across the US.
3. Measurements
In this study, the demographic data encompassed a range of variables including the child’s age, sex, education, employment status, language, family structure, and ethnicity. The independent variables in focus were family resilience including problem-solving, communication, strength recognition, and maintaining hope [12]. For problem-solving, participants were asked, ‘When your family faces problems, how often are you likely to work together to solve our problems?’ Similarly, for communication, the question was, ‘When your family faces problems, how often are you likely to talk together about what to do?’ Strength recognition was evaluated with the question, ‘When your family faces problems, how often do you know you have strengths to draw on?’ Lastly, the aspect of hopefulness was assessed through the question, ‘When your family faces problems, how often are you likely to stay hopeful even in difficult times?’ Responses to these family resilience questions were scaled from 1 (all of the time) to 4 (none of the time). For meaningful interpretation, scores were reversed, resulting in a scoring range for family resilience from 4 (lowest level of resilience) to 16 (highest level of resilience). The dependent variable in this study was the perceived well-being, encompassing both mental and physical health aspects. Participants were asked to rate their mental health with the question, ‘In general, how is your mental or emotional health?’ and their physical health with, ‘In general, how is your physical health?’ Response options for these questions ranged from 1 (excellent) to 5 (poor). To align with the interpretation that higher scores indicate better outcomes, these scores were also reversed. Consequently, the well-being score ranged from 2 (indicating the lowest level of perceived well-being) to 10 (representing the highest level of perceived well-being). The reverse scoring of both metrics does not alter the interpretation of the analysis but ensures that higher scores on both scales are indicative of better outcomes, simplifying comparisons and interpretations. Both family resilience and well-being measurements have been used in this survey annually since 2003 by the Maternal and Child Health Bureau in the US, underscoring their enduring utility and relevance in assessing maternal and child health outcomes.
4. Data Analysis
The analysis of the study data was conducted using the Statistical Package for Social Sciences (SPSS) software, version 27 (IBM Corp.). Descriptive analysis was used to present the socio-demographic data of the participants, including variables such as the child’s sex, language, employment, education, family structure, race, and caregiver’s age. To ensure the appropriateness of the statistical tests used, the normality of the data was assessed using the Kolmogorov-Smirnov test. To examine the relationship between family resilience and caregiver’s well-being, Spearman’s rank correlation test was used because data was not normally distributed. Cross-tabulation analysis was performed to examine the distribution of family resilience across the different age groups. Chi-square tests were used to assess the association between these age groups and family resilience and covariates. Next, linear regression analysis was conducted to assess the impact of family resilience on caregiver well-being in each age group, controlling for covariates such as language, employment status, and family structure. The significance level for all tests was set at the .05 level, aligning with standard practices in statistical analysis.
RESULTS
1. Correlation Between Family Resilience and Caregiver Well-being
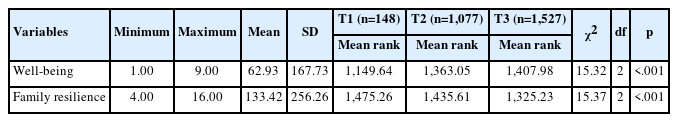
As shown in Table 1, the analysis revealed a moderate positive correlation between family resilience and caregiver’s well-being (r=.35, p<.001). This finding suggests that higher levels of family resilience are associated with better caregiver well-being among children with ADHD across different age groups.
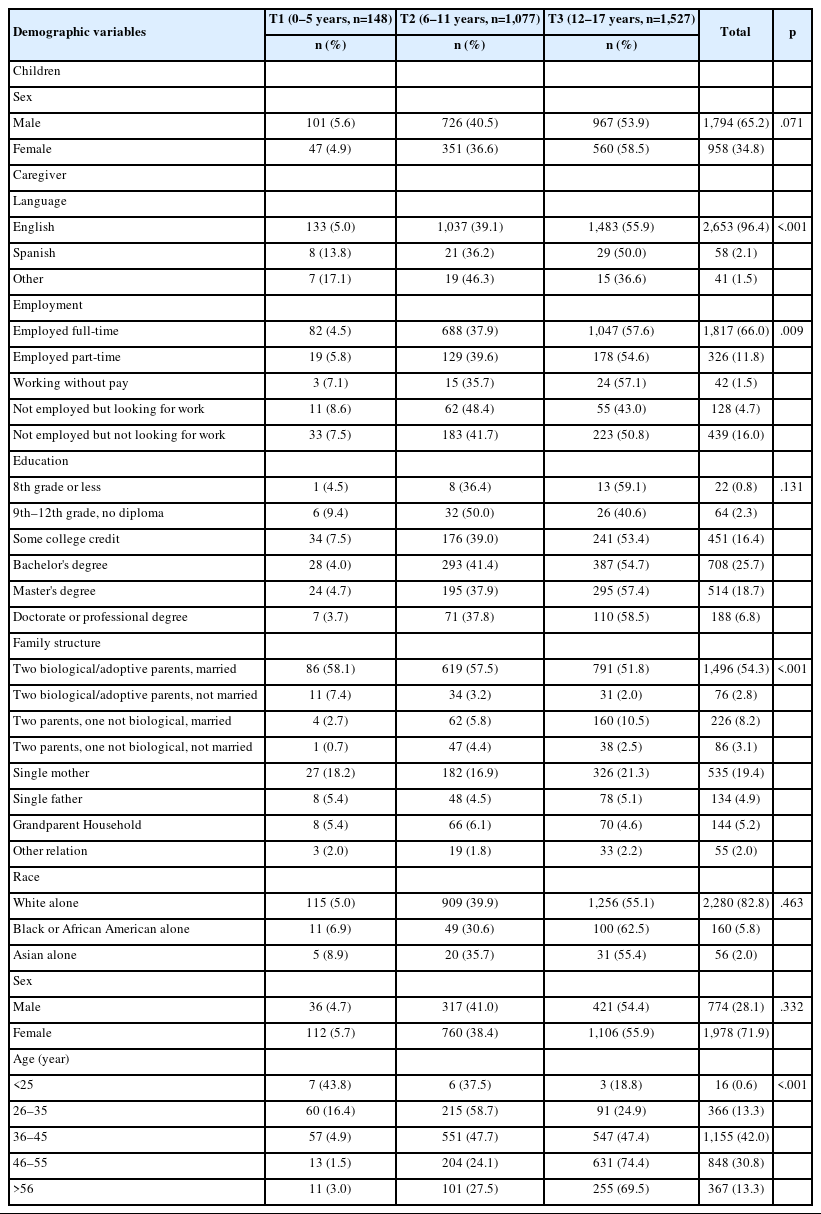
2. Demographic Characteristics
The demographic characteristics of children with ADHD and their caregivers are presented in Table 2. Predominantly, children in the study were male (65.2%), with the highest proportion in the 12–17 years age group. Caregivers were largely female (71.9%), especially in the oldest age group. English was the predominant language spoken by caregivers (96.4%). Employment status showed a majority of caregivers were employed full-time (66.0%), with the highest percentage in the 12–17 years age group. Educational attainment was diverse, with a bachelor’s degree being the most common (25.7%). The family structure was predominantly two biological/adoptive parents who were married (54.3%). Regarding race, a significant majority identified as white alone (82.8%). The age distribution of caregivers showed a concentration in the 36–45 years range (42.0%).
3. Non-parametric Test Analysis (Kruskal-Wallis) for Well-being and Family Resilience
The 12–17 years age group showed the highest well-being mean rank (1,407.98) but had the lowest mean rank for family resilience (1,325.23). From the chi-square test, language, employment, family structure, and caregiver’s age are associated with child’s age. For well-being and family resilience, based on Kruskall–Wallis, there is a difference among groups (Table 3).
4. Associations Between Family Resilience, Covariates, and Caregiver’s Well-being
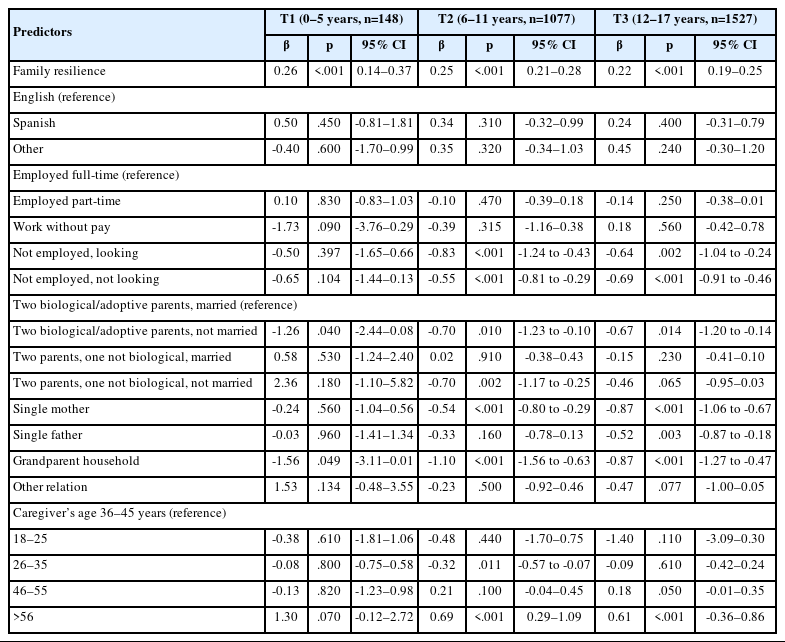
1) Age group T1
Controlling for covariates, family resilience was positively associated with the caregiver’s well-being in the T1 age group (β=0.26, p<.001), and it explains 25.2% of its variance (Table 4). For each standard deviation increase in family resilience, the caregiver’s well-being increased by 0.26 standard deviations. Among the significant covariates, living in a household with two biological or adoptive parents not currently married was negatively associated with the caregiver’s well-being (β=-1.26, p=.040). Additionally, residing in a grandparent household also showed a negative association (β=-1.56, p=.049).
2) Age group T2
In the T2 age group, family resilience continued to demonstrate a significant positive relationship with the caregiver’s well-being (β=0.25, p<.001), and it explains 21.1% of its variance (Table 4). Caregivers not looking for work (β=-0.55, p<.001) and those actively looking for work (β=-0.83, p<.001) were both negatively associated with the caregiver’s well-being. The family structure, particularly living in a grandparent household (β=-1.10, p<.001) and being in a household with two biological or adoptive parents not currently married (β=-0.70, p=.010), were negatively associated. Additionally, caregivers in the 26–35 age group (β=-0.32, p=.011) and those older than 56 years (β=0.69, p<.001) showed significant associations, with the older age group positively associated. Single-mother households were also negatively associated with the caregiver’s well-being (β=-0.54, p<.001).
3) Age group T3
For the T3 age group, family resilience again showed a significant positive association (β=0.22, p<.001), and it explains 22.1% of its variance (Table 4). Employment status, both for caregivers looking for work (β=-0.64, p=.002) and those not looking for work (β=-0.69, p<.001), was negatively associated with the caregiver’s well-being. The family structure, especially single-mother households (β=-0.87, p<.001) and grandparent households (β=-0.87, p<.001), and being in a household with two biological or adoptive parents not currently married (β=-0.67, p=.014), were all negatively associated with caregiver’s well-being.
DISCUSSION
The current study provides a comprehensive analysis of the relationships between family resilience, various covariates, and the caregiver’s well-being across different age groups. Family resilience constantly displays a positive impact on the caregiver’s well-being, while specific characteristics in the employment status, family structure, and caregiver’s age vary in all developmental ages.
In this study, family resilience has a positive impact on caregiver’s well-being in all children’s age groups. This implies its use is imperative in caring for children with ADHD. Family resilience revolves around the ability of families to recognize their strengths amidst adversity and to rebound from challenges [20]. Enhancing the proactive approach of families towards challenges and maximizing their capacity for problem-solving can significantly aid in their effective management [10], including in families with children diagnosed with ADHD.
In the T1 age group, family resilience was positively associated with the caregiver’s well-being (β=0.26, p<.001), indicating that higher levels of resilience correspond to more favorable outcomes. Similarly, in the T2 age group, family resilience remained a significant positive predictor (β=0.25, p<.001). The finding highlights resilience’s role in maintaining stability and positive outcomes, even as children grow older. In the T3 age group, family resilience continued to show a significant positive association (β=0.22, p<.001), reinforcing its importance across the lifespan. Family resilience was responsible for 25.2%, 21.1%, and 22.1% of the variation in caregiver well-being for the age groups 0–5, 6–11, and 12–17 years, respectively. The consistency of these percentages across different age groups highlights the sustained importance of family resilience throughout various stages of a child’s development. The T1 group employs family resilience slightly higher than other age groups. Family resilience tends to be more significantly employed during crisis periods, focusing on the development and preservation of supportive familial connections and the enhancement of family belief systems [21]. During that period, children are diagnosed with ADHD [22], which explains the use of family resilience in these early years. As children mature, the persistence of challenges in caring for children with ADHD necessitates that caregivers adapt by employing various coping strategies, including the seeking of social support [23]. Hence, collaborating with caregivers to enhance their coping strategies and social support networks presents a viable approach to strengthening resilience within all age groups [24].
In general, employment status, family structure, and caregiver’s age play a role in the well-being of caregivers. However, specific characteristics of these variables are different among age groups. In the youngest age group, T1, the well-being of caregivers and children is influenced by several key factors. The structure of the family plays a critical role, with biological/adoptive parents, not currently married showing a notable negative association (β=-1.26). This can be explained that parents who live together without being married tend to be younger, often less equipped for parenting roles, and have a higher likelihood of separating compared to those who are married [25]. This finding points to the potential difficulties faced by single-parent or separated families in this age group. Therefore, the patient’s age may be the reason for this difference. Interestingly, older caregivers (>56 years) demonstrate a positive impact on well-being (β=1.30), suggesting that older caregivers may have more resources, experience, or coping mechanisms. Moreover, younger caregivers might simultaneously face additional stress factors [20].
As children enter school age, the T2 age group presents distinct trends. The stress of unemployment or job-seeking remains significant, as shown by the negative associations of ‘not working, look for work’ (β=-0.83) and ‘not working, not look for work’ (β=-0.55). This underscores the impact of employment challenges on the well-being of caregivers with school-aged children. Single motherhood (β=-0.54) and grandparent-led households (β=-1.10) emerge as factors associated with lower well-being. This aligns with research findings that single mothers often experience reduced well-being due to the challenges of handling daily responsibilities on their own [17]. Mothers raising children alone are typically younger, do not have the support of a second parent, and experience lower levels of social support relative to caregivers in varied family structures [25]. Moreover, in grandparents-led family structures, financial difficulties can often occur, especially among those with lower incomes [26,27]. These grandparents are frequently faced with the economic burden of supporting both their grandchildren and their adult children. Distinct from the grandparent-led family structure, the trend of older caregivers experiencing better well-being continues in this age group, reinforcing the notion that age and accumulated life experience can positively influence caregiver well-being.
In the adolescent T3 age group, several factors significantly impact caregiver well-being. The consistent negative impact of unemployment or job-seeking is evident, highlighting the stress associated with these employment statuses in families of adolescents with ADHD. Challenges in non-traditional family structures are pronounced, with being biological/adopt parents not married, single mothers, single fathers and grandparent-led households showing significant negative impacts. This suggests that the complexities and demands of caregiving in these structures are particularly challenging during the adolescent years. This study also indicates that caregivers aged 36–45 years and above 56 years generally exhibit better well-being. A study from Taiwan demonstrated that long-term multigenerational caregivers, including those caring for grandchildren, report better self-rated health, higher life satisfaction, and fewer depressive symptoms [28], which aligns with the findings of the current research conducted in the US. This sense of contentment can be partially attributed to the adequacy of their social support networks and coping mechanisms [29]. Despite the geographical differences, the similarity in results between the two studies underscores the need for further research to explore this phenomenon across diverse cultural and national contexts.
Understanding family resilience with caregiver well-being across different age groups of children with ADHD is imperative, as highlighted by the findings of this study. The significance of this focus is further supported by other research, which reveals that family resilience scores in families with children diagnosed with ADHD are lower compared to those in families dealing with other chronic illnesses [30] and that the quality of life for caregivers of children with ADHD is lower than that of caregivers of children in general [31]. Given the distinct challenges of caring for children with ADHD, as highlighted by our study and further evidenced by comparisons with both healthy children and those with other chronic conditions, there emerges a pressing need for tailored interventions designed specifically to support families of children with ADHD.
This study carries significant implications for practice, education, and research. The specific implications for nursing practice in each age group are further elucidated below.
Nurses at public health centers or clinics should prioritize strategies that strengthen family resilience for caregivers of children aged 0 to 5 years by providing resources for stress management and family counseling, and by offering support to older caregivers that leverage their experiences while addressing potential physical health challenges. This is crucial for caregivers of children in this age group where family resilience has a significant positive impact on well-being. A study in Iran stands out for its emphasis on the necessity of training caregivers in problem-solving, anger management, and adaptability skills [5]. Furthermore, in response to the pandemic, telehealth or online parenting resources are proposed to increase the efficacy of family-based interventions [21].
For children aged 6 to 11 years, nurses need to focus on enhancing family communication skills, as well as providing targeted support for single mothers and older caregivers. Introducing programs that foster family bonding and effective communication is crucial [21] as children enter school age. Furthermore, education programs aimed at stress management for caregivers of children in this age group, which encompass training in communication skills, family resilience, emotional-focused family resilience techniques, and comprehensive reviews of effective stress management knowledge, have been shown to significantly enhance their caregiving abilities [32]. Also, nurses should focus on the unique challenges faced by single mothers and grandparents raising children, offering specialized support groups, resources for managing caregiving stress, and connections to community assistance programs. Recognizing the positive impact of older caregivers, nurses should offer health maintenance advice, support for managing chronic conditions, and resources to assist in caregiving responsibilities.
As children grow into adolescence, nurses need to facilitate training focused on stress management and family resilience that addresses the changing dynamics of families with teenagers. Additionally, nurses should provide support for single mothers, single fathers, and grandparent-led households, recognizing the unique challenges these caregivers face. Family therapy can significantly benefit parents by promoting more adaptive family resilience and enhancing their ability to manage the challenges associated with their child’s condition in the family context [33]. Moreover, targeted interventions for single mothers, single fathers, and grandparent-led households are essential. These interventions should include adolescent behavioral management strategies, mental health support, and resources for navigating the challenges of raising teenagers.
In education, the incorporation of knowledge about family resilience and caregiver well-being into nursing curricula is essential. This integration not only prepares nursing students with essential skills but also ensures that practicing nurses receive ongoing education to keep updated with the latest research findings.
In research, a qualitative study is needed to refine and expand upon the findings of this study. This approach will allow for a more nuanced understanding of the differences in family resilience and caregiver well-being across various age groups. Additionally, longitudinal studies would offer valuable insights into the changes in caregiver well-being and family resilience strategies as children with ADHD age.
In nursing practice, despite varying factors, unemployment consistently emerges as a key predictor of reduced well-being among caregivers across all age groups. Those unemployed are prone to financial challenges. In this context, nurses can serve as crucial advocates, communicating these insights to policymakers to encourage the establishment of regulations and financial support for families with children who have ADHD, especially during their period of unemployment.
The limitation of this study is its cross-sectional nature, as derived from the NSCH data. Due to this design, the study is unable to establish a causal relationship between the observed variables. This means that while the study can identify associations between caregiver’s well-being, family resilience, and child age groups, it cannot conclusively determine cause-and-effect relationships. Moreover, due to the use of secondary data, the variables explored are limited to those available in the NSCH dataset, potentially overlooking other important aspects of family resilience. Additionally, as the research was conducted within the US, its applicability to other countries or cultural contexts may not be warranted, limiting the generalizability of the findings beyond the US demographic.
Despite its limitations, this study has significant strengths. One of the most notable is the large number of respondents involved, which enhances the reliability of the findings. Using national data collected through a representative design is another major strength. This approach ensures that the sample accurately reflects the broader population, thereby increasing the validity of the conclusions drawn from the study.
CONCLUSION
This study reveals that caregiver’s well-being in children with ADHD is influenced by a complex interplay of factors that vary across different developmental stages of the child. Family resilience proportionally contributes to this outcome. Also, various characteristics of the caregiver’s employment status, family structure, and caregiver’s age impact both positively and negatively on the caregiver’s well-being. These insights highlight the need for distinct family resilience interventions tailored to different developmental stages. Addressing these specific requirements can significantly enhance caregiver well-being and positively influence family dynamics with children diagnosed with ADHD. Future studies could benefit from a qualitative methodology to delve deeper into the nuances of well-being and family resilience among children with ADHD at different ages, thereby facilitating the improvement of developmentally appropriate interventions. Additionally, conducting similar studies in different cultural contexts would be invaluable in understanding the influence of cultural factors on family resilience and caregiver’s well-being.
Notes
Authors' contribution
Conceptualization: all authors; Data collection, Formal analysis: all authors; Writing-original draft: all authors; Writing-review and editing: all authors; Final approval of published version: all authors.
Conflict of interest
No existing or potential conflict of interest relevant to this article was reported.
Funding
None.
Data availability
Please contact the corresponding author for data availability.
Acknowledgements
None.