Healthcare coaching program for youth with type 1 diabetes in South Korea: a pilot study
Article information
Abstract
Purpose
This pilot study aimed to assess the feasibility, preliminary efficacy, and effects of a mobile app healthcare coaching program developed based on self-regulation theory among youths with type 1 diabetes.
Methods
A mixed-method design was utilized. Participants were randomly assigned into intervention (n=23, 12-week coaching program) or control groups (n=16, usual care). Pre- and post-intervention assessments included self-efficacy, diabetes management behavior, and health outcomes (quality of life, depression, and HbA1c). Quantitative data were analyzed with SPSS/WIN ver. 26.0. The narrative information from the participants in the healthcare coaching program underwent content analyzed.
Results
The intervention group had significantly lower depression scores (t=2.57, p=.014) than the control group. No significant differences were observed in self-efficacy, diabetes management behavior, and health outcomes between the two groups. The average frequency of health behavior monitoring per week among the participants was 1.86±1.60. The qualitative findings indicated that participants perceived improved diabetes self-management with the intervention; however, challenges during vacations, dietary control difficulties, and a lack of disease awareness were identified.
Conclusion
The healthcare coaching program improved psychological aspects for youth with type 1 diabetes. Further research is needed to develop and implement mobile app interventions aimed at enhancing compliance with diabetes management in pediatric and adolescent populations.
INTRODUCTION
In 2022, out of the global population of 8.75 million individuals with type 1 diabetes (T1D), 1.52 million were under the age of 20 years. It is estimated that 108,200 children and adolescents under 15 years are diagnosed with T1D each year [1]. The Centers for Disease Control and Prevention (CDC) reported a notable surge in the diagnosis of T1D in the United States from 2017 to 2020. The overall increase was approximately 30.0%, with a particularly significant rise in the incidence rates among adolescents aged 10 to 14 years reaching 33.5%, and children aged 5–9 years, where the rate spiked to 37.0% [2]. Against this backdrop, glycemic control remains a substantial challenge, particularly for youth with T1D.
T1D treatment involves daily insulin administration, regular glucose monitoring, education, and support [3]. Optimal glycemic control is crucial to reduce the risk of diabetes-related complications and mortality in patients with T1D [4,5]. Despite this, self-management in youth with T1D is notably poor, with 73.0% of youths having an HbA1c of 8.0% or higher [5]. Additionally, approximately 55.0% of youths with T1D engage in alcohol consumption, which negatively influences diabetes management and growth [6]. This underscores the need to address the significant challenges youths with T1D face and to enhance their suboptimal diabetes management.
Adolescence is a period marked by physical hormonal changes, rapid growth in height and weight, increased metabolism, elevated insulin requirements, and psychological and cognitive shifts [7]. This phase involves various life changes, including academic and social aspects, which can interfere with effective diabetes management. Consequently, youths with T1D encounter additional complexities during this transitional time [8]. Effective self-management is crucial during this period, as poorly controlled diabetes leads to the development of acute and chronic complications [3].
Given that 95.0% of teens own a cell phone and 67.0%–95.0% use social media almost constantly, the use of mobile technology is a promising method to engage youths with T1D in their self-care [9]. Recently, mobile apps for diabetes management have been developed and utilized to enhance diabetes self-management. A meta-analysis examining mobile app interventions for T1D highlighted their effectiveness in improving HbA1c [10]. Alfonsi et al. [11] employed a mobile app for carbohydrate counting to calculate insulin doses for injections, which resulted in a reduction in HbA1c, and 43.0% of users continued to use the app after program completion. According to a report by Barnes et al. [12], 75.0% of adolescents and nearly 69.0% of parents of young patients expressed willingness to use mobile apps to manage diabetes. Thus, adopting a mobile application as a self-management tool for youth with T1D is expected to aid in achieving long-term diabetes control, reducing complications, and enhancing overall health.
Recently, a mobile app program was developed to assist individuals with type 2 diabetes (T2D) in managing their condition through the self-regulation model [13]. Participants can input, oversee, and manage multiple health behaviors—exercise, diet, blood glucose, and medication—while receiving automated personalized feedback and goals from the collected app data. We anticipate that youths with T1D can utilize the developed mobile app to monitor their self-management, as well as obtain personalized feedback and goals based on their history. This approach is expected to aid in achieving long-term diabetes control, reducing the risk of developing complications, and enhancing their overall health.
Accordingly, we aimed to explore the feasibility of a self-regulation theory-based healthcare coaching program delivered through a mobile app for youths with T1D. Our goal was to assess the program’s feasibility and preliminary effects and to investigate participants’ experience through qualitative data. Throughout this study, we investigated the following hypotheses:
H1. The intervention group will have higher levels of self-efficacy for diabetes self-management.
H2. The intervention group will have higher levels of health behaviors.
H3. The intervention group will have higher levels of health outcomes compared to the control group.
METHODS
Ethics statement: This study was approved by the Institutional Review Board (IRB) of Pusan National University Yangsan Hospital (No. 05-2022-021). Informed consent was obtained from all participants.
1. Study Design
This study was a concurrent mixed methods research where the qualitative and quantitative data were collected and analyzed during the same timeframe. Our mixed methods research included a pilot randomized controlled trial to evaluate the feasibility of a self-regulation theory-based healthcare coaching program via a mobile app for youths with T1D (CRIS identifier: KCT0008734). The reporting of this study was based on the Consolidated Standards of Reporting Trials (CONSORT) 2010 statement [14].
2. Study Setting
The study was conducted in Pusan National University Children’s Hospital, Yangsan, South Korea from February 8, 2022 to February 6, 2023.
3. Quantitative Study
1) Participants
The inclusion criteria for participants were as follows: (1) aged 10 to 18 years; (2) receiving insulin treatment (including multiple doses of insulin, insulin pump, or those utilizing continuous glucose monitoring) following a diagnosis of T1D; (3) obtained consent from both participants and parents/legal guardians; (4) capable of operating an Android smartphone; and (5) absence of medical conditions that would impede physical activity. The exclusion criteria encompassed individuals with: (1) cognitive impairments that could impact questionnaire completion; (2) a history of psychiatric disorders or current use of psychotropic medication; and (3) severe coexisting conditions requiring treatment beyond T1D. Prior research suggests a minimum of 25 participants per group for a pilot study with a moderate effect size (0.5) [15]. Therefore, considering the dropout rate [16], a total of 60 patients were recruited (26 and 21 in the intervention and control groups, respectively) in a 3:2 ratio using an Excel-generated list (ver. 2019; Microsoft). Initially, 47 participants agreed to participate, 26 and 21 of whom were assigned to the intervention and control groups, respectively. Three participants in the intervention group dropped out during the intervention due to a decline and a failure to make contact, and five participants in the control group declined to participate the study at the post-test. A total of 39 participants (intervention group=23, control group=16) were included in the final analysis (Figure 1). Participants and researchers were not blinded to the random assignment.
2) Measurements
(1) General and disease-related characteristics
Participant characteristics, including age, sex, grade level, alcohol consumption, and smoking habits, were collected via structured questionnaires. Disease-related information included diabetes duration, height, weight, blood glucose measurement type, insulin injection methods, occurrences of diabetes-related complications leading to hospitalization, and blood glucose levels during the interview.
(2) Self-efficacy for diabetes self-management
Self-efficacy was measured using the Korean version of the self-efficacy for diabetes self-management (SEDM) scale [17]. Authorization for the use of the Korean version of the SEDM scale [17] was obtained from the Korean translator; however, attempts to contact the original developer of the scale for permission were unsuccessful. The scale comprises ten items assessing self-confidence in diabetes self-management. An example item is “Do you think you can make healthy food choices when you go out to eat?”. Responses varied from 0 (not at all confident) to 10 (very confident). The total self-efficacy scores were computed by averaging the 10-item scores, with higher scores indicating enhanced self-efficacy. The Cronbach’s ⍺ was .90 at the time of tool development [18]. In the study by Boo et al. [17], conducted with Korean children with diabetes, the reported Cronbach’s ⍺ was .87, while in this study it was .91.
(3) Health behaviors
Health behaviors in this study include the diabetes management behaviors and dietary intake. Diabetes management behaviors were measured using the Korean version of diabetes management behavior scale (DMBS) [17]. Authorization for the use of the Korean version of the DMBS was obtained from the Korean translator; however, attempts to contact the original developer of the scale for permission were unsuccessful. The scale comprises 36 items with four sub-domains (daily preventive behaviors, modifying diabetes management plan, intervention behaviors in the past 7 days, and other diabetes management behaviors), and assesses the ability to perform behaviors for diabetes management. Responses vary from 0 (never) to 4 (always) and from 0 (occurred 0 times) to 5 (occurred 5 times). Due to the various responses for each item, all items were converted to a scale ranging from 0 to 1. The total score was calculated as the mean of each item and ranged between 0 and 1, with. higher scores indicating better diabetes control. In the study by Boo et al. [17], conducted with Korean children with diabetes, the reported Cronbach’s ⍺ was .86, while in this study it was .89.
Dietary intake over a 3-day period was measured using the 24-hour recall method [19]. Utilizing the Computer Aided Nutritional Analysis Program 4.0 (CAN Pro 4.0; The Korean Nutrition Society) from the Korean Nutrition Society, the mean intake for each food group was computed over three days based on United States Department of Agriculture (USDA) MyPlate guidelines [20]. Caloric intake calculations employed standard weight, activity levels, and daily exchange units per food group from Dudek’s textbook [21]. To determine the actual intake compared to the recommended serving size, we computed the individual's actual intake ratio by dividing the consumed serving sizes by the recommended serving sizes and multiplying the result by 100.
(4) Health outcomes
Health outcomes in this study include quality of life, depression, and HbA1c. Quality of life was measured using the PedsQL 4.0 generic core scales, which were acquired and utilized under the authorized permission of Mapi Research Trust (http://www.pedsql.org). The scale comprises 23 items tailored for adolescents aged 13 to 18 years and measures four sub-domains of functioning: physical, emotional, social, and school. Responses, collected on a 5-point Likert scale, were reverse-scored and linearly transformed to a 0–100 scale (0=100, 1=75, 2=50, 3=25, 4=0), with higher scores indicating a better quality of life. Cronbach’s ⍺ was .90 at the time of tool development [22] and .94 in this study. Depression was measured using the Korean-translated BDI-II depression scales for adolescents [23] to evaluate symptoms over the preceding two weeks. The scales were acquired and utilized with permission from Korea Psychology Corporation, which provided the scoring system and categorization of depression severity: 0–13 (minimal), 14–19 (mild), 20–28 (moderate), and 29–63 (severe) [24]. The scale consists of 21 items rated on a severity scale of 0–3, with the exception of two items that are rated on a scale of 0–6. Cronbach’s ⍺ was .89 at the time of tool development [23] and .85 in this study. Participants visited outpatient clinics approximately every 3 months, and HbA1c measurements were conducted every 3 to 6 months. HbA1c values were collected from medical records, and the nearest HbA1c value to the data collection date was obtained from the chart, considering the frequency of patient visits and HbA1c measurements.
3) Data collection
Quantitative data was collected between February 8, 2022, and February 6, 2023. The researcher (DL) collected data from participants face-to-face when potential participants visited outpatient clinic. Parents and youths were provided with an explanation of the research objectives, procedures, and their right to withdraw from the research at any time. Those who voluntarily agreed to participate in the research signed consent forms. All collected data were treated anonymously and stored on the researcher’s personal computer with a password. Documented materials were kept in a locked cabinet and, in accordance with the IRB, will be discarded after a retention period. The intervention group completed a 12-week program, while the control group did pre-surveys and post-surveys over the same 12-week period. Both groups received $5 gift cards upon completing data collection.
4) Data analysis
Data analysis was performed using SPSS version 26.0 (IBM Corp.) with a significance level set at p≤.05. Homogeneity between intervention and control groups at pre-test was assessed using the χ2-test, the Fisher's exact test, and independent t-test for the characteristics of the participants and dependent variables. The normality of dependent variables was assessed using the Kolmogorov-Smirnov test. Most dependent variables showed a normal distribution in the Kolmogorov-Smirnov analysis (p>.05), except of diabetes management behavior, food intake (dairy and fruit intake), and sub-domains of quality of life (physical and psychosocial health), and HbA1c. Within-group differences in the dependent variables were evaluated using paired t-tests or Wilcoxon signed-rank tests. Specifically, variables such as self-efficacy for diabetes self-management, dietary intake (grains, protein, and vegetables), and quality of life, which demonstrated a normal distribution, were examined through paired t-tests. Wilcoxon signed-rank tests were employed for the remaining variables that did not follow a normal distribution. Group differences in the dependent variables between pre- and post-tests were analyzed using either the independent t-test or Mann–Whitney U test, depending on the normality of the data. Variables, including self-efficacy for diabetes self-management, dietary intake (grains, protein, and vegetables), quality of life, and depression, which exhibited a normal distribution, were evaluated using independent t-tests. For the remaining variables that did not follow a normal distribution, Mann–Whitney U tests were employed.
4. Qualitative Study
1) Participants
Participants in the intervention group who were willing to participate in the interview and understood the study's subject, objectives, methodology (including the necessity of qualitative interviews and audio recordings) participated in the qualitative study at the post-test. Participants were informed of their right to discontinue or withdraw from participation at any time without negative consequences.
2) Qualitative interviews
The researcher (DL) conducted qualitative interview. A semi-structured questionnaire was used to inquire about participants' feelings toward the healthcare coaching program and whether their diabetes habits had changed since engaging in the program. The interviews were conducted using the following main questions: “How was participating in the healthcare coaching program?”, “What efforts have you made to manage diabetes during participating in the program?”, and “Have there been people or environments that were helpful or hindered your diabetes management while participating in the program?”. Interviews were conducted after participants’ outpatient clinic visits in an empty medical office in the hospital, either with the child alone or with the child and their parent. The interviews lasted 10 to 15 minutes. All interviews were recorded and the researcher (DL) transcribed the recordings by carefully listening to participants' spoken words and cross-checking by re-listening to the recordings.
3) Data analysis
Transcribed records were analyzed using an inductive approach and followed the content analysis method outlined by Elo and Kyngäs [25]. Participants were provided comprehensive information about the research, including its purpose, assurances of confidentiality, absence of compensation or risk, and the right to refrain from answering or withdraw at any point. Interviews, which were recorded with the option to pause, were transcribed and assigned random anonymized numbers for confidentiality. In the preparation phase, data were thoroughly understood by reviewing transcribed records. In the categorization phase, sentences representing participants' experiences were selected as the analytical unit through open coding, and similar content was grouped to create categories and sub-categories. The results were reviewed by a nursing professor for credibility, and the researcher's neutrality supported objectivity and ensured confirmability of the results. The integration of qualitative and quantitative findings was conducted through narrative and contiguous approach [26]. Using the approach, we analyzed and reported the quantitative findings from the first half and the qualitative findings concerning participants' feelings toward the healthcare coaching program or their changes in diabetes habits in the second half.
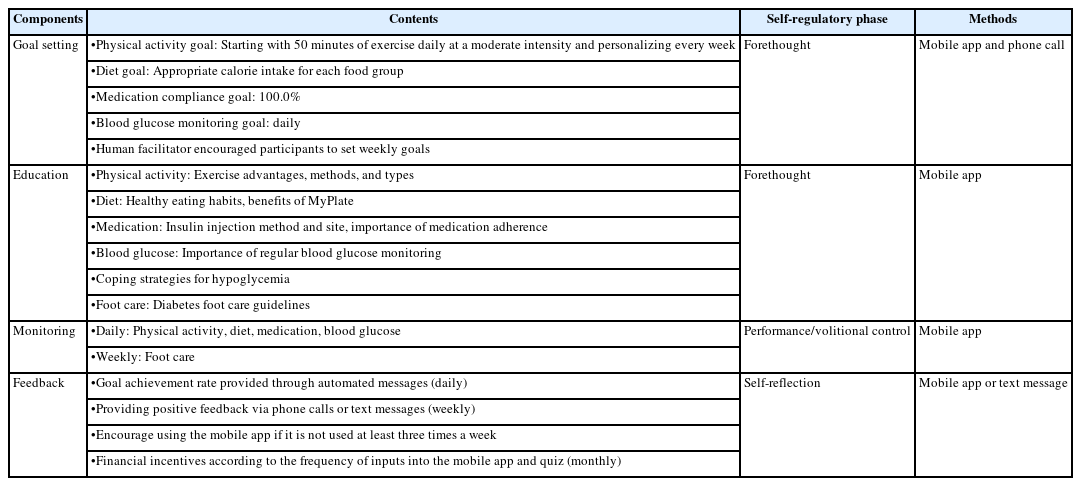
5. Healthcare Coaching Program
The healthcare coaching program in this study was based on the Automated Personalized Self-Care program [13], which was originally developed for T2D and modified for youths with T1D (Table 1). It included goal setting, education, monitoring, and feedback. The program allowed participants to monitor physical activity, diet, blood glucose, and medication following MyPlate and physical activity guidelines [27]. Weekly messages, calls supported goal tracking, and education content were delivered via cartoons, videos, and materials from Pusan National University Yangsan Hospital. Daily monitoring included blood glucose, diet, physical activity, medication, and insulin injections, and achievement rates were displayed. Average frequency of health behavior monitoring per week among the participants was 1.86±1.60. Weekly feedback and incentives were provided for engagement, and the researcher offered positive feedback to encourage app use via calls or messages.
RESULTS
1. Quantitative Results
1) Demographic characteristics
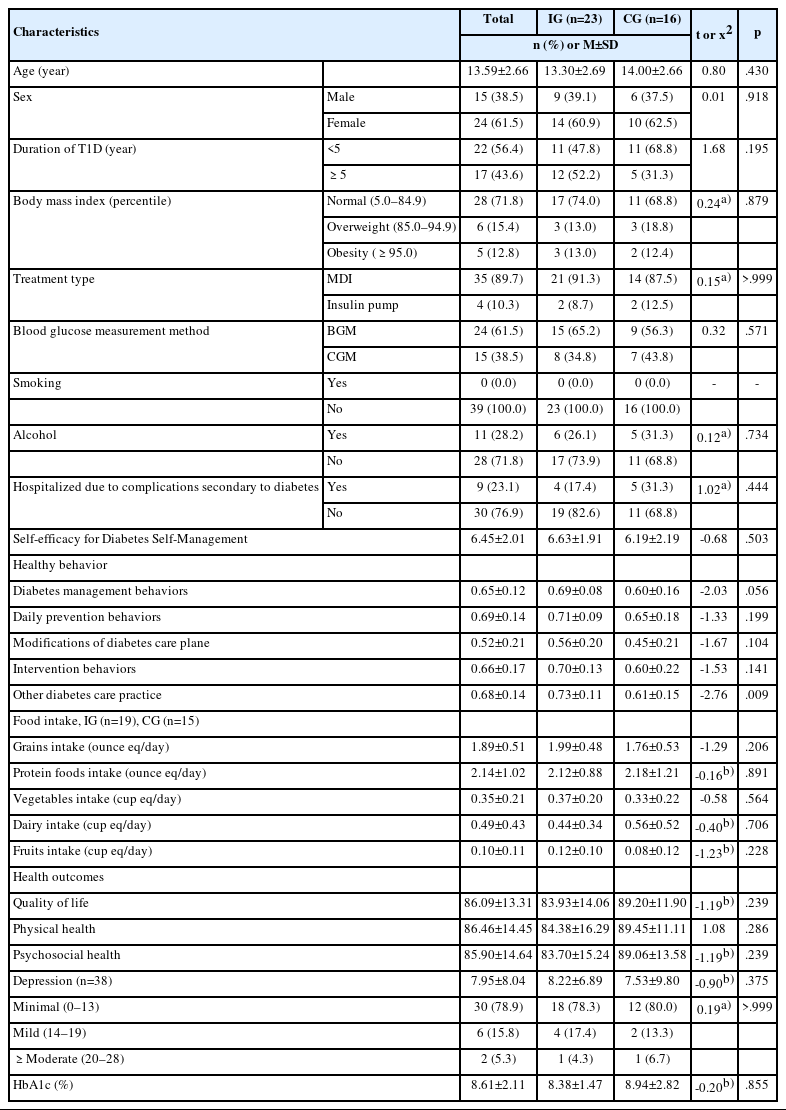
A total of 70 participants were assessed for eligibility. A total of 47 were enrolled, with 26 in the intervention group and 21 in the control group. During the intervention, four from each group withdrew, resulting in a final sample of 39 participants (Figure 1). The mean age of the participants was 13.59±2.66 years, with 61.5% being female. Participants' mean HbA1c exceeded 8.6%. Approximately 56.4% of participants had been diagnosed with T1D for less than five years, and 28.2% had an experience of alcohol drinking. The majority used multiple doses of insulin (89.7%) and monitored their blood glucose levels with a blood glucose meter (61.5%). Nine participants (23.1%) had been hospitalized due to diabetes-related complications.
2) Test of baseline homogeneity of variables between groups
For the pre-test variables, there were no significant differences in self-efficacy for diabetes self-management, diabetes management behaviors, food intake, and quality of life (both overall and its sub-domains), depression, and HbA1c, indicating homogeneity between groups at pre-test. However, a significant difference between groups was observed in other diabetes care practice, a sub-domain of diabetes management behavior (Table 2).
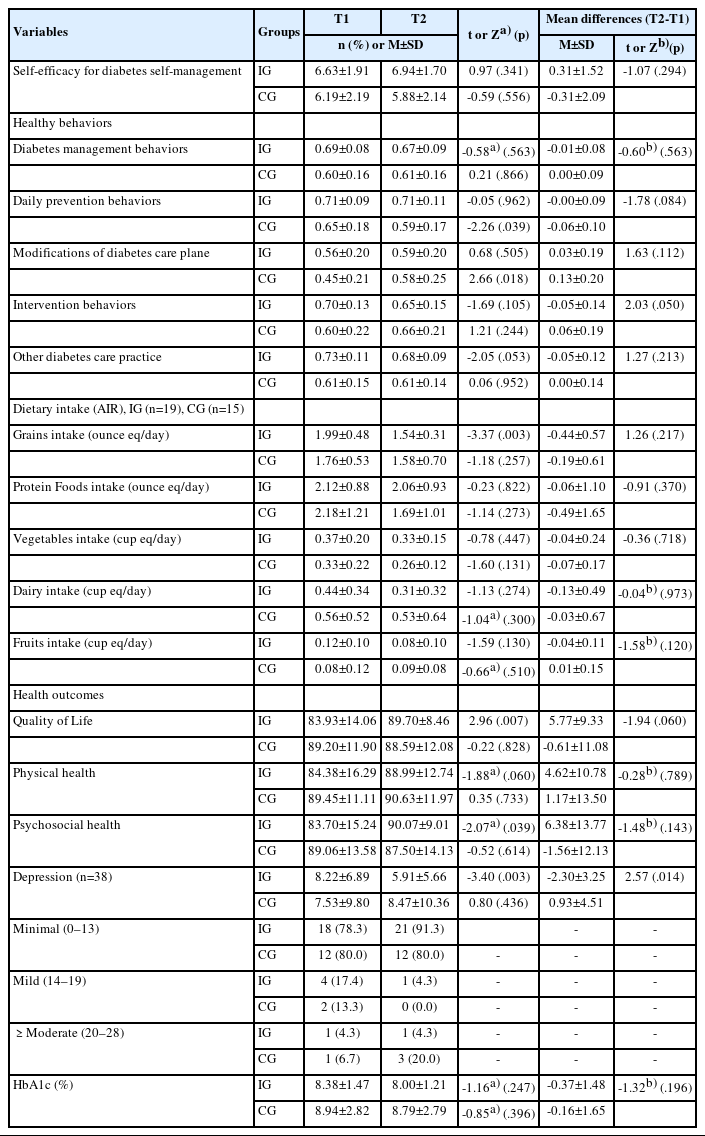
3) Hypothesis testing
There was no harm or unintended effects in each group. Table 3 summarizes the intervention outcomes. The between-group difference in self-efficacy for diabetes self-management was not statistically significant (t=-1.07, p=.294), so H1 was rejected. Similarly, the between-group difference in diabetes management behavior was not statistically significant (Z=-0.60, p=.563), so H2 was rejected. However, in the within-group analysis, the control group exhibited significant differences in sub-domains of the diabetes management behaviors—a significant decrease in daily preventive behaviors (t=-2.26, p=.039) and a significant increase in modification of the diabetes care plan (t=2.66, p=.018). Moreover, in the within-group analysis, the intervention group showed a significant decrease in grain intake (t=-3.37, p=.003). H3 was partially supported. The between-group difference in quality of life was not statistically significant (t=-1.94, p=.060). However, in the within-group analysis, the intervention group exhibited a significant increase in overall quality of life (t=2.96, p=.007) and in the quality of life sub-domain of psychosocial health (Z=-2.07, p=.039). The between-group difference in depression was statistically significant (t=2.57, p=.014) and the intervention group exhibited a significant decrease in depression compared to the control group. In the within-group analysis, the intervention group exhibited a significant decrease in depression (t=-3.40, p=.003). The between-group difference in HbA1c levels did not show significant changes (Z=-1.32, p=.196).
2. Qualitative Results
A total of 22 participants from the intervention group participated in narrative interviews, leading to the identification of three themes and 11 sub-themes (Table 4).
1) Theme 1: Diabetes management challenges
(1) Sub-theme 1a: The challenges of diabetes management due to surrounding conditions/environment
This sub-theme shows how participants faced challenges in managing their diabetes due to external circumstances such as schoolwork and vacations.
“I've been trying to work out... I used to work out a lot. During the semester, I get busy and don't do as much...” (Participants 9)
(2) Sub-theme 1b: Choosing between temptation and restraint
This sub-theme indicates that participants would put diabetes management on the back burner due to difficulties with food moderation and wanting to hang out with friends.
“I thought I had to type in the mobile app even if it was annoying. I thought it was fun to play with my friend, but it didn't work. I got really into playing.” (Participants 22)
(3) Sub-theme 1c: Hassle of diabetes management and lack of time due to busy schedule
This sub-theme emphasizes that participants struggled with mobile app diabetes management due to laziness and annoyance.
“I'm a bit of a nuisance, so over time, I think, ‘I have to type now,’ but after I exercise and shower, I forget that I have to type. There were many times when I was chatting after midnight and realized that I didn't type, but I didn't type.” (Participants 4)
(4) Sub-theme 1d: Failure to alert for illness
This sub-theme emphasizes that diabetes complications did not develop immediately, indicating a lack of awareness of the disease.
“Knowing about my condition... That's crucial. Right now, I'm not quite aware because I feel the same whether my blood sugar is high or low.” (Participant 12)
2) Theme 2: Positive change
(1) Sub-theme 2a: Reflecting on and improving their diabetes management after participating in the program
This sub-theme indicates that the feedback participants’ received after entering the mobile app made them reflect on and improve their diabetes management.
“When I put it in the app, I saw I was having too much meat and not enough veggies. So, I attempted to cut down on meat and include more vegetables. Also, when dining out, I aimed to opt for vegetable dishes.” (Participant 36)
(2) Sub-theme 2b: Setting and reaching goals to manage your diabetes
This sub-theme indicates that participants found it helpful to set goals to manage their diabetes.
“I would type it into the mobile app and check it, and sometimes my workout would go up to 90%, and I was so happy to see that, I slept so well.” (Participant 42)
(3) Sub-theme 2c: Increased awareness of diabetes management
This sub-theme emphasizes that participants gained insights into their diabetes management through program engagement using a mobile app.
“The first one is...now I know things that I didn't know, so I'm trying to be a little bit more careful with that...for example, I'm trying to be careful with my feet now, like you said I can't hurt my feet anymore...so I'm trying to be careful with my feet.” (Participant 42)
3) Theme 3: Advantages and limitations of using mobile apps to manage diabetes
(1) Sub-theme 3a: The convenience of a mobile app
This sub-theme indicates that the mobile app is easy to use and that the diabetes management feedback is helpful.
“I don't need to carry around a notebook or anything. It's easier to track everything on my phone now. I can view what I've eaten, monitor the quantity, and identify when I've gone over the limit, making things a bit more convenient.” (Participant 36)
(2) Sub-theme 3b: Difficulties with the types of food that can be entered in the mobile app
This sub-theme highlights app limitations, such as a restricted food variety and challenges in finding specific types of food, such as snacks and foreign dishes.
“Entering food into the app was confusing. There are so many types of food... I didn't know how to record what I ate because it wasn't in the app.” (Participant 4)
DISCUSSION
This study aimed to evaluate the feasibility and preliminary effects of a healthcare coaching program while exploring participants’ experiences through qualitative data. The study included youths with an average age of 13.6 years, of whom 61.5% were female, and 61.5% monitored their blood sugar with a glucometer. Notably, 28.2% were classified as overweight or obese, and 28.2% reported alcohol consumption. Considering the mean age of the youths in this study (13.59±2.66 years), the alcohol consumption rates was notably high. For the youths with T1D and a mean age of 21.3 years [6], the alcohol consumption rates was much higher, reaching 55.0%. Additionally, the rate of overweight or obese adolescents with T1D in the previous study [5] were higher than that in this study, reaching 38.8%. Alcohol use was associated with worsened HbA1c levels, high lipid levels, and concurrent smoking [6]. Moreover, overweight status was a significant risk factor for compromised HbA1c levels [5]. Consequently, it is advisable to actively promote education and practices in diabetes management for youths with T1D starting from an early age.
The participants in this study reported slightly higher than the medium levels of self-efficacy in diabetes self-management, diabetes management behavior, and quality of life, representing 6.45±2.01, 0.65±0.12, and 86.09±13.31, respectively. The levels of HbA1c was 8.61%±2.11%, which exceeds the target range of <7.5%. Participants reported minimal levels of depression, with a score of 7.95±8.04. Soufi et al. [28] reported a similar level of self-efficacy (6.80±1.60), and HbA1c (8.40%±1.30%) score for participants in their study compared with those in our study. Participants in our study with higher baseline self-efficacy showed strong association with adherence and diabetes management, which aligns with the finding of another study deploying a pathway model [29]. Strong self-efficacy might help adolescents manage T1D despite its challenges and enable them to improve self-management and HbA1c levels. This suggests the need for diabetes management and education in Korean youths with T1D and increased attention to improve their psychosocial and clinical factors.
The healthcare coaching program effectively alleviated depression among youths with T1D but failed to demonstrate significant improvements in diabetes self-efficacy, health behaviors (including diabetes management and dietary intake), and health outcomes (such as quality of life and HbA1c levels). In the control group, the levels of depression did not show significant changes between the pre- and post-tests, whereas in the intervention group, there was a significant decrease in depression levels at the post-test. The coaching program in this study was grounded in self-regulation theory, which has been proven to be an effective strategy in alleviating depressive symptoms among adolescents with T1D. Participants in the intervention group mentioned during the interviews that setting weekly goals and receiving feedback through a mobile app were beneficial for managing diabetes. A meta-analysis assessing the effectiveness of self-regulation theory-based interventions with youths also reported their effectiveness in improving self-regulation and reducing depression [30]. Given the strong correlation between depression and low quality of life [17] as well as elevated levels of HbA1c [29], these findings underscore the significance of self-regulation theory-based interventions in reducing depression and their potential impact on improving HbA1c control in youths with T1D. Self-regulation can serve as an effective strategy for improving glycemic control and managing negative emotions (e.g., depression and anxiety) that may overwhelm youths with T1D.
The healthcare coaching program in this study did not significantly improve self-efficacy, diabetes self-management, or HbA1c levels in youths with T1D. A meta-analysis [10] of randomized clinical trial studies on mHealth in people with T1D showed no significant change in HbA1c reduction in adolescents, but a sub-analysis found a significant change in adults. This is consistent with the results of several previous studies [31]. Management of T1D in adolescents is complex, influenced by various factors, including physical activity, diet, growth, insulin resistance, and psychological elements [3,7]. Youths with T1D face significant psychological and cognitive changes, which present challenges in diabetes management and are influenced by factors such as schoolwork and friendships [12,28,29]. The participants in this study might have had fewer self-management skills than adults and a less comprehensive understanding of health education. Poor adherence in diabetes management can impact HbA1c level [5]. In a study by Lansing et al. [32], where incentives were provided for achieving diabetes management goals, goal attainment ranged from 80.0% to 93.3%. As a result, significant improvements in self-monitoring of blood glucose and HbA1c levels were observed. Interventions utilizing mobile apps demonstrate promise for diabetes management in adolescents. However, they require refinement to address this age group’s specific needs. Accordingly, further research to identify effective self-management interventions is necessary.
The program in this study did not lead to significant improvements in dietary intake (grains, protein, vegetables, dairy, and fruit), as there were no notable group differences observed at the post-test. However, significant differences were observed within the intervention group. Specifically, grain intake significantly decreased from pre-test to post-test among participants in the intervention group. Given the association of grain intake with HbA1c levels and insulin injection doses [4,11], the mobile app’s potential to facilitate dietary modifications appears promising. During interviews conducted after program completion in this study, participants in the intervention group expressed their efforts to understand and refine their dietary habits through graph feedback for food entries. However, in the intervention group, only three participants demonstrated high adherence to the intervention by entering their blood glucose levels five times per week, which contrasts with an average of one entry per week for the entire intervention group. Goyal et al. [31] observed a significant reduction in HbA1c levels among a subgroup that monitored their blood glucose more than five times a day, indicating a relationship between monitoring and adherence. In chronic conditions such as T1D in youths, adherence has been linked to self-management [29]. Hence, interventions aimed at enhancing adherence should be developed to prevent diabetes complications.
The dietary assessment of youths with T1D revealed excessive intake of grains and protein surpassing the recommended amounts and indicated insufficient consumption of fruits, dairy products, and vegetables. This finding aligns with Seckold et al.’s research [4], which showed that only 50% of T1D youths met the recommended fruit and vegetable intake levels. These results underscore the necessity to enhance dietary habits among youths with T1D. A meta-analysis [33] revealed a strong correlation between consuming 35 g of dietary fiber daily and a significant decrease in premature mortality ranging from 10.0% to 48.0%. This fiber intake level also led to notable improvements in HbA1c, lipid profiles, and body weight. Moreover, a sufficient intake of dietary fiber promotes a smoother post-prandial glucose profile, which emphasizes the importance of regular consumption of fruit and vegetables in the diet of youths with T1D.
This study holds significance as it employs a mixed methods research approach to assess the effectiveness of a mobile app healthcare coaching program for adolescents with T1D in South Korea. The research combines quantitative methods to evaluate program efficacy with qualitative methods exploring participants' experiences. This study confirms the effectiveness of an intervention based on self-regulation theory in improving depression. However, several limitations should be noted, including low adherence among adolescents with T1D. Adherence might influence self-efficacy, health behaviors (diabetes management behavior and dietary intake), and health outcomes (quality of life, depression, and HbA1c). Therefore, it is necessary to evaluate the intervention’s effectiveness, considering adherence as a key factor. Furthermore, the intervention had a small number of participants, so it is necessary to recruit a large sample to validate the intervention’s effectiveness. Additionally, the limited variety of foods that could be entered in the dietary input of the mobile app posed challenges in providing comprehensive dietary feedback. Based on the above discussion, several future suggestions emerge. First, we propose future research to develop strategies to enhance adherence and to evaluate the effectiveness. Second, we recommend expanding the participant pool to validate the intervention’s effectiveness. Third, we suggest increasing the variety of foods that can be entered into the mobile app for the intervention. Finally, the dietary analysis of youths with T1D was not conducted by food group; hence, we recommend analyzing by food group in the future.
CONCLUSION
This study aimed to evaluate the feasibility and preliminary effects of a healthcare coaching program while exploring participants’ experiences through qualitative data. The program successfully reduced depression in youths with T1D but did not significantly improve self-efficacy, health behaviors (including diabetes management and diet), or health outcomes (quality of life and HbA1c levels). Participants had a diet low in dairy, vegetables and fruits but high in grains and proteins. App feedback improved diabetes management behavior, but inconsistent usage due to laziness, annoyance, and dietary entry issues resulted in low compliance. However, using the app itself was not problematic. The findings underscore the necessity of diabetes management interventions that develop strategies to enhance youths’ adherence to diabetes management. Future studies should expand the variety of foods that can be entered into the mobile app to improve ease of use. Additionally, considering incentives for achieving each goal could be beneficial in enhancing adherence to the intervention.
Notes
Authors' contribution
Conceptualization: all authors; Data collection, Formal analysis: all authors; Writing-original draft: all authors; Writing-review and editing: all authors; Final approval of published version: all authors.
Conflict of interest
No existing or potential conflict of interest relevant to this article was reported.
Funding
This work was supported by a 2-Year Research Grant of Pusan National University.
Data availability
Please contact the corresponding author for data availability.
Acknowledgements
None.