Weight status in survivors of childhood acute lymphocytic leukemia in South Korea: a retrospective descriptive study
Article information
Abstract
Purpose
This study investigated weight status in survivors of childhood acute lymphocytic leukemia (ALL) and identified related factors.
Methods
A retrospective review of the electronic medical records of survivors of childhood ALL (n=230) was conducted. We analyzed the survivors' characteristics, including sex, age, weight status at diagnosis, central nervous system involvement, risk classification, length of treatment, radiation therapy, and hematopoietic stem cell transplantation. Analysis of variance and the chi-squared test were applied to investigate influencing factors.
Results
The weight status distribution was as follows: 23 individuals (10.0%) were classified as underweight, 151 individuals (65.7%) were healthy weight, and 56 individuals (24.3%) were overweight/obese. Age at diagnosis (F=10.03, p<.001), weight status at diagnosis (x2=43.41, p<.001), and risk classification (F=10.98, p=0.027) showed significant differences among the weight status groups. Survivors who were older at diagnosis and those in the very high-risk category had a higher likelihood of experiencing underweight status during their survivorship, while survivors who were overweight/obese at diagnosis were more likely to remain overweight/obese at the time of survival.
Conclusion
Considering the potential health implications related to an unhealthy weight status in survivors of ALL, it is imperative to undertake early identification and implement interventions for at-risk individuals.
INTRODUCTION
Acute lymphocytic leukemia (ALL) is a type of cancer that originates in the bone marrow and affects the body's ability to produce healthy blood cells. It is the most common type of cancer diagnosed in children, accounting for one-fifth of all childhood cancers. In 2020, 175 children were newly diagnosed with ALL, and the annual incidence of ALL was 27.4 cases per million children aged 0 to 14 years in South Korea [1].
Children with ALL endure rigorous treatment. However, it is no longer a terminal prognosis. The majority of children who have suffered from cancer can now be cured. According to Korea's cancer statistics in 2020, the 5-year relative survival rate for patients with childhood cancer was 85.7% [1]. This marks a significant increase from 56.8% in 1995. The remarkable improvements in survival rates have led to a growing population of childhood cancer survivors with extended lifespans. As the size of the childhood cancer survivor group increases, there is a greater need to pay attention to their overall health problems.
Although treatment developments and supportive care have improved chances for survival in patients with childhood cancer, these improvements have led to long-term health-related outcomes (i.e., late effects). These late effects include physical, mental, and social problems, as well as secondary cancer. They are caused by the cancer or by its treatment and occur months or years after treatment has ended. Studies have shown that, among survivors of childhood cancer, 60% to more than 90% had at least one chronic health condition and 20% to 80% had a severe, life-threatening, or disabling condition in adulthood, including cardiovascular disease (CVD), endocrine disorders, permanent alopecia, growth impairment, infertility, and cognitive dysfunction [2-6]. Therefore, an understanding of late complications is of utmost important.
Unhealthy weight status is a well-known major risk factor for several chronic diseases. In the general population, underweight is associated with an elevated risk of infection [7], infertility [8], CVD [9], and fracture [10]. The underweight population in Korea has been shown to have a heightened risk of mortality [11]. As the degree of underweight becomes more severe, the risk of stroke, CVD, and mortality increases [12]. Furthermore, underweight not only has detrimental effects on physical health but also on mental health. People who are underweight report diminished psychological health [13] and increased depressive symptoms [14]. Underweight status increases the health vulnerability of survivors. Underweight survivors of childhood cancer have a significant risk of decreased heart function [15]. In addition, they have a 2.8-time higher mortality rate than survivors with healthy weights [16]. Even though underweight status is a significant concern for survivors of childhood cancer, it has been studied less than obesity.
Obesity is a well-known contributor to many health problems. As a late effect, obesity further exacerbates the risk of chronic health conditions in survivors who are already susceptible. Furthermore, obesity is associated with increased mortality and a greater risk of cancer recurrence in survivors [17].
Previous studies have shown associations between the characteristic indicators of obesity in childhood cancer survivors and factors related to the tumor, the patient, and the treatment. The finding that survivors of ALL have a higher body mass index (BMI) than the general population [18] is considered a tumor-related factor. In previous studies, patient-related factors included sex, baseline BMI, and age at diagnosis. Female survivors tended to have a higher prevalence of obesity than male survivors [19-21]. A younger age at diagnosis was associated with a higher risk of being overweight or obese [22,23]. Survivors who were overweight/obese at diagnosis have an elevated risk of remaining obese after treatment completion [22-25]. Treatment-related factors included the length of treatment and the use of radiation therapy. The length of cancer treatment appears to be a significant risk factor for obesity; a study found that as the length of treatment increased by 1 year, survivors had a 1.6 times higher risk of obesity [26]. It is also widely accepted that radiation therapy increases the risk of obesity during survivorship. Several studies found that cranial radiation therapy was associated with excessive weight gain in survivors [21,23,27,28].
A better understanding of the characteristics associated with an unhealthy weight is crucial for identifying high-risk groups and providing interventions. Notably, however, there is a global lack of research investigating the characteristics of underweight in survivors of childhood cancer. Although it has been confirmed that both underweight and overweight/obesity play a significant role in the health of survivors, most studies have focused on overweight/obesity. Therefore, this study aimed to identify the factors associated with both underweight and overweight/obesity in survivors of ALL.
Weight status is influenced by various factors, and these factors vary from one country to another. Therefore, it is crucial to ascertain country-specific characteristics. Most studies have been conducted abroad, and their applicability to Korean survivors is limited. The paucity of Korean studies dedicated to this subject have primarily investigated the factors associated with overweight/obesity. Moreover, the conclusions from these studies regarding the correlations between cranial irradiation and increased BMI have been inconsistent [29,30]. Therefore, this study investigated the characteristics of weight status using Korean data.
The purpose of this study was to examine weight status in survivors of childhood ALL, specifically 1) to determine the prevalence in each weight status category and 2) to identify the characteristics associated with each weight status category. The ultimate goal of this study was to identify groups at risk for problems related to weight status, who could then receive early interventions that promote their health throughout life.
METHODS
Ethics statement: The Institutional Review Board (IRB) of Seoul National University Hospital (No. 2209-111-1359) reviewed this study and designated it as an exempt research study.
1. Study Design, Setting, and Sample
This was a retrospective descriptive study conducted in a pediatric oncology clinic at a tertiary hospital in Korea. This study followed the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guidelines [31]. Children diagnosed with ALL who had survived more than 5 years were eligible for this study. The inclusion criteria were: 1) children who are diagnosed between ages 1 and 18 years, 2) children who were diagnosed with ALL for the first time according to the International Classification of Childhood Cancer, 3) children who were diagnosed between January 1, 2005, and June 30, 2018, and 4) children who were alive 5 years after diagnosis. Therefore, data on the survivors spanned the period from January 1, 2010, to June 30, 2023. The exclusion criteria were: 1) children with a diagnosis that could affect body weight prior to their cancer diagnosis, (e.g., diabetes and Down syndrome), 2) foreign patients, 3) children who had already initiated treatment at other hospitals, and 4) children currently undergoing treatment for relapse or secondary cancer. Figure 1 elucidates the procedure of sample selection.
2. Measurements
1) Weight status
Weight status was evaluated using BMI. BMI is a person's weight in kilograms divided by their height in meters squared (kg/m2). It is a cost-effective and straightforward way to screen for weight categories. Because age-, sex-, and nationspecific BMI values exist for children and adolescents, it is recommended to use BMI percentiles. A BMI percentile compares an individual's weight to that of their peers in the same age and sex group and determines whether a child' s BMI falls within a healthy range. Underweight is defined as below the 5th percentile, while a healthy weight is between the 5th and 85th percentiles. Overweight is between the 85th and 95th percentiles, while obesity is above the 95th percentile. The classification of weight status in this study is based on the 2017 Korean National Growth Charts for children and adolescents [32]. The baseline weight status at the time of diagnosis refers to the measured BMI value obtained just before the initiation of cancer treatment. Weight status at survivorship refers to the measured BMI value obtained at the hospital visit closest to the 5-year mark after diagnosis.
2) Patient-related factors
Patient-related factors included sex, age at diagnosis, and weight status at diagnosis. Weight status was categorized by BMI percentiles.
3) Tumor-related factors
In the context of ALL, tumor-related factors included: 1) central nervous system (CNS) involvement of leukemic cells and 2) risk classifications. Patients with ALL were assigned to standard-risk, high-risk, and very high-risk groups based on the criteria, and their treatment approaches varied according to risk group. The classification criteria included the child's age at diagnosis, initial white blood cell (WBC) count, subtype of ALL, extramedullary manifestations, chromosomal abnormalities, and response to induction therapy. In the research setting, each group was classified according to the following criteria [33]:
• Standard-risk group: age 1 to 9 years, WBC <50,000/μL
• High-risk group: age ≥10 years, WBC ≥50,000/μL, Tcell lineage, or history of steroid use.
• Very high-risk group: chromosome count <45, induction failure (bone marrow blasts ≥5% on induction day 28), mixed lineage leukemia gene rearrangement, early T-cell precursor ALL, biphenotypic ALL, or Philadelphia chromosome-positive ALL.
4) Treatment-related factors
Treatment-related factors included the length of treatment and the use of radiation therapy or hematopoietic stem cell transplantation (HSCT). The length of treatment was calculated in months. In cases where patients did not undergo HSCT, the treatment duration was calculated from the initiation of treatment until the final bone marrow examination. For those who underwent HSCT, it was calculated as 1 year after transplantation.
3. Data Collection and Procedure
Electronic medical records (EMRs) were reviewed during June 2023. The collected data were stored in encrypted files to ensure that only authorized researchers had access to them. This study was considered minimal-risk research, and the informed consent process was waived.
4. Data Analysis
Statistical analyses were performed using SPSS version 29.0 (IBM Corp.). The quantitative variables included age at diagnosis and length of treatment. The categorical variables included sex, weight status at diagnosis, risk classification, CNS involvement, radiation therapy, and HSCT. Descriptive statistics were initially used to summarize the quantitative variables as means and standard deviations and the categorical variables as counts and percentages for each classification. Second, chi-square tests were conducted for the categorical variables, and one-way analysis of variance (ANOVA) was performed for the continuous variables. The study investigated differences in patient-, treatment-, and tumor-related factors using the chi-square test and ANOVA.
RESULTS
1. Sample Characteristics
General characteristics of the ALL survivors (n=230) are presented in Table 1. The sex distribution was comparable, with 126 males and 104 females. The mean age at diagnosis was 82.93 months. At the time of diagnosis, the average BMI was 17.03 kg/m2, and the median BMI percentile was 46.70.

Demographic Statistics of the Survivors of Childhood Acute Lymphocytic Leukemia at a Single Tertiary Hospital in Seoul, South Korea, 2010-2023 (N=230)
The average age of survivors 5 years after diagnosis was 143.66 months. At that time, the average BMI was 19.48 kg/m2, and the median BMI percentile was 66.15. An increase in the median BMI percentile was observed from diagnosis to survival.
2. Prevalence Rates of Weight Status among Survivors
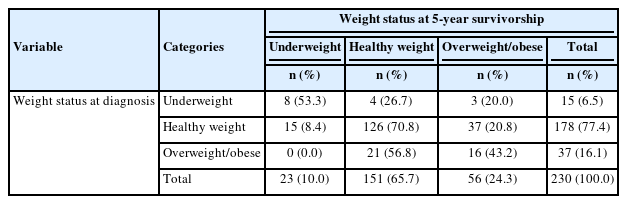
Weight status was categorized into three groups: 1) underweight, 2) healthy weight, and 3) overweight or obese. To compare the weight status of patients with ALL at the time of diagnosis and at 5 years of survival, a contingency table was constructed. At the time of diagnosis, 15 individuals (6.5%) were classified as underweight, 178 individuals (77.4%) as healthy weight, and 37 individuals (16.1%) as overweight/obese. At 5 years, 23 survivors (10.0%) were classified as underweight, 151 survivors (65.7%) as healthy weight, and 56 survivors (24.3%) as overweight/obese. An analysis of survivors whose weight status changed from diagnosis to survival showed that 15 (8.4%) transitioned from healthy weight to underweight, while 40 (20.7%) transitioned from underweight or healthy weight to overweight/obese (Table 2).
3. Differences between the Underweight, Healthy Weight, and Overweight/Obese Groups
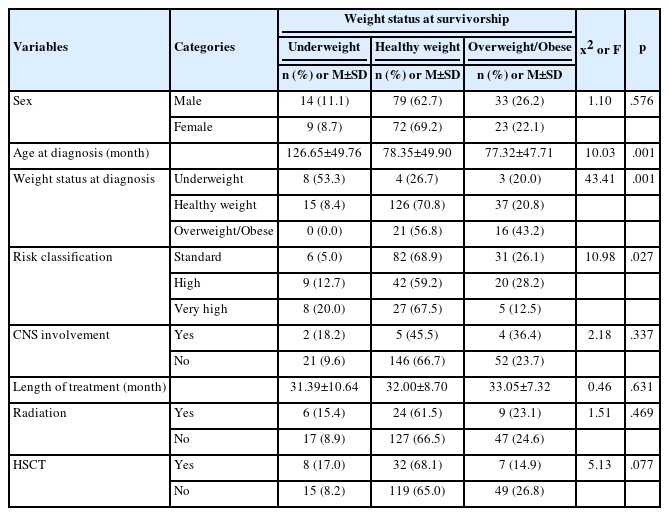
To examine the differences in patient-related characteristics based on weight status at survival, variables including sex, age at diagnosis, and weight status at diagnosis were analyzed (Table 3). The results revealed statistically significant differences in age at diagnosis (F=10.03, p<.001) and weight status at diagnosis (x2=43.41, p<.001). Conversely, there were no statistically significant differences in the relationship of sex to weight status at survival. Subsequent post-hoc analyses were conducted to further explore the variables that showed significant differences. These analyses showed that the underweight group had a higher age at diagnosis than the healthy weight status and risk classification (F=10.98, p=.027). In the very high-risk group, eight individuals (20.0%) were classified as underweight, which was a higher proportion than the standard-risk group with six individuals (5.0%) and the highrisk group with nine individuals (12.7%). The higher-risk group classifications had higher proportions of underweight individuals. Conversely, in the very high-risk group, five individuals (12.5%) were categorized as overweight/obese, a lower proportion than the standard-risk group with 31 individuals (26.1%) and the high-risk group with 20 individuals (28.2%). No significant differences were observed for CNS involvement.
Differences between the Underweight, Healthy Weight, and Overweight/Obese Groups among Survivors of Childhood Acute Lymphocytic Leukemia (N=230)
An analysis of the treatment-related factors (length of treatment, radiation therapy, and HSCT) based on weight status at survivorship indicated no significant differences across all three variables.
DISCUSSION
This study was a descriptive retrospective analysis of the weight status and related characteristics of childhood ALL survivors in a single center setting in Seoul, South Korea. Using data from EMRs, this study revealed differences in age, weight status at diagnosis, and risk classification among the weight status groups. However, no significant differences were observed in terms of sex, CNS involvement, treatment duration, radiation therapy, or HSCT.
At the time of diagnosis, 178 patients (77.4%) were classified in the healthy weight range, but this group decreased to 151 patients (65.7%) at the 5-year survival mark. This indicated an increased prevalence of unhealthy weight conditions, including underweight and overweight/obese survivors.
In this study, 56 survivors (24.3%) were overweight/obese, while 23 survivors (10.0%) were underweight. According to a cohort study of childhood cancer survivors in the United States (US), 6.2% were underweight, 53.2% were a healthy weight, 27.7% were overweight, and 12.8% were obese [34]. Our study demonstrated a higher prevalence of underweight individuals and a lower prevalence of overweight and obese individuals than the US study. A Swiss survivor cohort study that examined the weight distribution among leukemia survivors reported proportions of 6% underweight, 68% healthy weight, and 26% overweight/obese [35]. Although the prevalence rates for the healthy weight and overweight/obese groups were similar, the prevalence of the underweight group was notably higher in our study. Our review of previous studies conducted in South Korea revealed a lack of research on the proportion of underweight survivors. The prevalence of overweight/obesity among survivors of all types of childhood cancer, as reported in the studies by Shin et al. [29] (17.2%) and Sohn et al. [30] (17.3%), was lower than the prevalence observed in our study.
An intriguing finding in this study was the high proportion of underweight individuals among survivors. According to the 2021 National Health Statistics in South Korea, the proportion of children and adolescents who were reported as underweight, overweight, and obese were 5.1%, 9.8%, and 19.3%, respectively [36]. When compared to the general population, the prevalence of overweight/obesity among childhood cancer survivors was similar to that of the national average. However, the rate of underweight individuals was nearly double. Previous research has predominantly focused on overweight/obesity in childhood cancer survivors, but the results of this study highlight the importance of addressing underweight status among survivors in Korea. Further investigation into this aspect of childhood cancer survival is needed.
In this study, those in the underweight group were older at the time of diagnosis than the healthy and overweight/obese groups. Previous studies focused on the relationship between younger age and the increased risk of obesity [22,23]. However, in this study, we also investigated the relationship between age and underweight status. Patients with ALL who are 10 years old and older are classified as high-risk and receive intensified treatment. This can lead to reduced nutritional intake and decreased physical strength due to nausea and vomiting. Dupuis et al. [37] demonstrated that, as age increases and treatment intensity rises, the risk of nausea and vomiting also increases in the standard-risk group of ALL. In addition, it has been noted that the use of antiemetic agents among pediatric patients with acute myeloid leukemia increases with age [38].
The weight status at diagnosis was also significantly different among weight groups. A significant number of survivors in our study maintained their initial weight status. Brown et al. [23] also observed that a higher BMI z-score at diagnosis was associated with overweight/obesity during survival. Razzouk et al. [22] further supported our results, reporting that overweight/obesity at diagnosis was associated with a 9.2-times higher risk of being overweight/obese during survival when compared to a healthy weight group. Furthermore, while previous studies focused on the obesity outcomes of patients who were obese at diagnosis [22-25], our study provided further evidence of the risk of remaining or becoming underweight among survivors who were underweight at diagnosis. In conclusion, weight status at the time of diagnosis influences weight status during the survival period. We emphasize the importance of early attention and intervention in the unhealthy weight groups at the time of diagnosis. Further research is also needed to identify the characteristics of children who transition from the healthy weight group to an abnormal weight group.
The risk classifications in this study demonstrated significant differences in weight status among the survivors. The very high-risk group exhibited a higher prevalence of underweight individuals and a lower prevalence of overweight/obese individuals than the standard and high-risk groups. Zhang et al. [25] found that survivors of childhood ALL in the high-risk group showed a decrease in BMI z-scores during treatment when compared to the standard-risk group, indicating an increased likelihood of being underweight. Hence, it is important to contemplate the risk of underweight among the very high-risk group. The higher proportion of underweight survivors in the very high-risk group may be attributed to their aggressive treatment, including high-intensity chemotherapy and HSCT.
In many previous studies, radiation therapy was found to increase the risk of overweight/obesity in survivors of ALL [21,23,27,28]. However, our study found no significant differences in the proportion of individuals who received radiation therapy among the different weight groups. This finding is consistent with the results of a study conducted in Korea by Shin et al. [29]. The lack of significant results between the two variables can likely be attributed to a decrease in the utilization of radiation therapy. Radiation therapy not only contributes to external changes such as skin fibrosis and alopecia but also plays a role in cognitive impairment. These side effects have a detrimental impact on quality of life for long-term survivors. Therefore, intrathecal chemotherapy is currently being used more frequently as an alternative to radiation therapy.
Children who survive ALL face numerous health issues during their extended lifespan. Abnormal weight, including underweight or overweight/obesity, adds an additional burden to these already vulnerable individuals. This study identified the characteristics of survivors with abnormal weight, providing a basis for early identification of high-risk groups and raising awareness about this issue. This study highlighted the importance of maintaining a healthy weight from the time of diagnosis. Patients and their families must be made aware of the impact of abnormal weight status on health early on and provided with interventions to maintain a healthy weight.
Providing interventions for health promotion is crucial in helping these individuals lead healthier lives in their extended survivorship. Currently, in South Korea, the management of childhood cancer survivors primarily revolves around medical consultations and screening programs. While the Cancer Survivor Support Service has led to the establishment of support centers that offer health promotion and social reintegration services, there are only three centers dedicated to childhood cancer survivors nationwide, and the services provided remain insufficient [39]. Traditionally, nurses have been instrumental in delivering effective interventions for health promotion. Therefore, based on the findings of this study, they can also play a significant role in providing effective interventions for achieving and maintaining a healthy weight in survivors of childhood cancer.
This study had some limitations due to its analysis of secondary data. First, there were limitations in the variables studied. Unhealthy weight status is associated with various factors, but this study focused on disease-related variables since the data were collected from EMRs. Consequently, additional confounding characteristics, such as family factors, were not investigated.
Furthermore, this was a single-center study based on data from a university hospital in Seoul, South Korea. The hospital is a tertiary care hospital, which typically serves as a referral center for patients with complex and severe medical conditions and attracts those seeking more advanced medical treatment than might be provided at other healthcare facilities. As a result, there were limitations in external validity and sample size. Therefore, multicenter studies at the national level are needed to validate this study.
CONCLUSION
The findings of this study can be utilized to assess the weight status of survivors of childhood ALL and identify individuals at higher risk of developing an unhealthy weight status. In this study, the proportion of underweight individuals among survivors was higher compared to the general population. Moreover, children diagnosed at an older age and those categorized in the very high-risk group were at an elevated risk of being underweight during their survivorship. Conversely, children who were overweight or obese at the time of diagnosis typically continued to be overweight or obese throughout their survivorship.
Among its strengths, this study examined the weight status of childhood ALL survivors in South Korea and explored their related characteristics. Describing unhealthy weight status as a distinct singular characteristic is difficult as it is associated with multiple factors, including country-specific characteristics. Therefore, it is crucial to conduct further studies focused on Korean survivors, such as this study, to identify related factors and to develop and implement interventions that promote a healthy weight status among Korean survivors of childhood cancer.
Notes
Authors' contribution
Conceptualization: all authors; Data collection, Formal analysis: Yeongseon Kim; Writing-original draft: Yeongseon Kim; Writing-review and editing: all authors; Final approval of published version: all authors.
Conflict of interest
No existing or potential conflict of interest relevant to this article was reported.
Funding
None.
Data availability
Please contact the corresponding author for data availability.
Acknowledgements
None.