Choi and Bang: Health-related quality of life in children with epilepsy: a concept analysis
Abstract
Purpose
This study aimed to conduct a concept analysis of health-related quality of life in children with epilepsy to promote conceptual clarification and facilitate mutual understanding of the concept.
Methods
Walker and Avant's concept analysis method was adopted.
Results
Health-related quality of life in children with epilepsy consists of six attributes: health status, inner strength, close relationships, resource-rich community, social acceptance, and changeability. According to the ecological system paradigm, these attributes are structured into five dimensions: organism, microsystem, macrosystem, exosystem, and chronosystem. These dimensions provide a comprehensive approach to the relationship between children with epilepsy and their environment. Epilepsy and interactions with multilevel ecological systems that are directly and indirectly related to children with epilepsy precede the concept, followed by positive and negative affective responses.
Conclusion
The findings of this study may support effective communication in various practice settings, thereby contributing to the health and well-being of children with epilepsy, as well as the development and expansion of interventions to improve their health-related quality of life.
Key words: Child; Epilepsy; Health; Quality of life
INTRODUCTION
According to the 2016 Global Burden of Disease collaboration, the disease burden of epilepsy is 13.5 million disability-adjusted life years (DALYs), accounting for more than 0.5% of the total global DALYs [ 1]. Epilepsy exhibits distinctive epidemiological characteristics, with a high incidence and prevalence in younger age groups. Approximately one child out of 150 is diagnosed with epilepsy during the first 10 years of life [ 2], and the prevalence of active epilepsy—defined as having one or more seizures within 5 years or requiring anti-epileptic medications—peaks in children aged 5 to 9 years [ 1]. Pediatric epilepsy is a complex neurological chronic condition accompanied by physical, cognitive, psychological, behavioral, educational, and social developmental difficulties, as well as unpredictable and uncontrollable seizures [ 3]. Additionally, unlike other chronic diseases, epilepsy has persistent negative perceptions because of historically prevalent misconceptions and prejudices [ 4], resulting in psychosocial problems, such as inferiority, stigma, and low self-esteem, in children with epilepsy that affect various aspects of their lives [ 3, 5]. Research in health care for patients with chronic diseases has recently focused on improving the health-related quality of life (HRQOL) during illness, moving beyond the alleviation of symptoms, as the survival rate and life expectancy of patients with chronic diseases have increased because of advances in medical technology [ 6]. As part of this movement, the Sustainable Development Goals announced by the United Nations in 2015 have brought changes in global health policy, and countries have assessed HRQOL to "ensure a healthy life and promote well-being". The Healthy People 2020 project in the United States focused on improving the quality of population health by introducing HRQOL as a major indicator for monitoring national health agendas along with general health status, health disparities, and social determinants of health [ 7]. South Korea's National Health Plan 2020 identified people's health levels and gaps by measuring HRQOL in the Korea National Health and Nutrition Examination Survey and Community Health Survey to evaluate the overarching goals of extending healthy life expectancy [ 8]. HRQOL provides useful descriptive information on children's health status, facilitates the identification of children at different levels of morbidity, and enhances the understanding of the disease experience from the child's perspective [ 9]. Despite the broad nature of the concept, there is universal agreement that HRQOL is subjective and changes over time [ 10]. However, at the same time, the meanings of existing concepts have been muddled due to a lack of fundamental understanding and clear identification of the unique attributes of groups. However, the attributes of HRQOL can vary greatly depending on the significant events experienced by individuals throughout life stages, groups, cultures, and countries [ 10], requiring a nuanced understanding and insight into the use of concepts. Therefore, this study aimed to perform a conceptual analysis of HRQOL in children with epilepsy to promote conceptual clarification and develop a better understanding of HRQOL in this population.
METHODS
Ethics statement: This study was a conceptual analysis of the healthrelated quality of life in children with epilepsy and was therefore exempt from institutional review board approval.
1. Study Design
This study is a conceptual analysis exploring the concept of HRQOL in children with epilepsy using the basic principles of conceptual analysis proposed by Walker and Avant [ 11]. Walker and Avant's [ 11] concept analysis methodology has been used in nursing to identify and specify the semantic structures of undefined or unclear phenomena or concepts. The methodology consists of eight steps: (1) select a concept, (2) determine the aims or purposes of the analysis, (3) identify all uses of the concept, (4) determine the defining attributes, (5) construct a model case, (6) construct additional cases (borderline, related, and contrary cases), (7) identify antecedents and consequences, and (8) define empirical referents. This study followed the criteria of the Preferred Reporting Items for Systematic reviews and Meta-Analyses extension for Scoping Reviews (PRISMA-ScR) checklist [ 12].
2. Data Collection and Analysis
To explore the nature of the concept, dictionaries and literature in various disciplines were investigated. Using the terms "epilepsy", "children", and "HRQOL", the literature was searched in RISS, DBpia, CINAHL, and PubMed. Studies were included if they were (1) written in Korean or English, (2) scholarly peer-reviewed, (3) available as full-text, and (4) published between 2000 and 2021. This search period was selected because HRQOL began to draw attention in 2000 as the U.S. Department of Health and Welfare included "improving quality of life" as an indicator to achieve overarching national goals in Healthy People 2000.
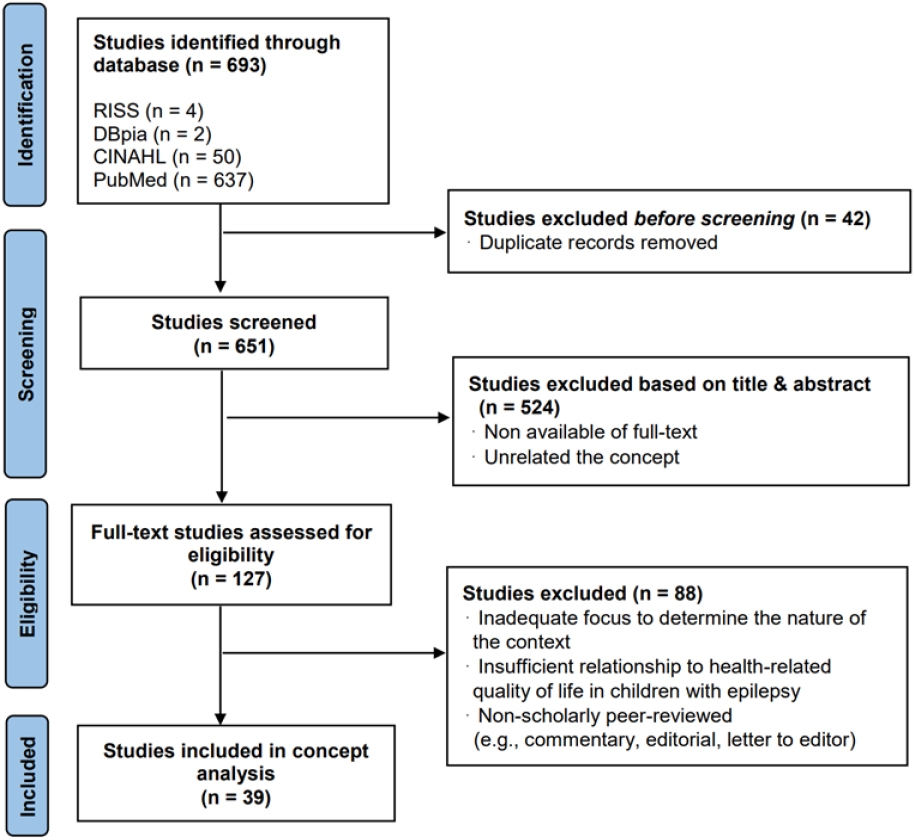
In total, 693 studies were identified in the search process. After eliminating duplicate studies, screening was performed by two researchers independently to control for selection bias. Studies were excluded if they (1) lacked conceptual focus or (2) were irrelevant to the research purpose. Finally, 39 studies were included in the concept analysis ( Figure 1).
RESULTS
1. Identifying all Uses of the Concept
1) Dictionary definitions of the term "health-related quality of life"
HRQOL does not appear as a term in any dictionary. Thus, the term was divided into "health" and "quality of life". According to the Standard Korean Dictionary [ 13], "health" means "mentally and physically unscathed and strong, or such a state". The Britannica Dictionary [ 14] defines "health" as (1) "the condition of being well or free from disease", (2) "the overall condition of someone's body or mind", and (3) "the condition or state of something". In Taber's Medical Dictionary [ 15], "health" is defined as (1) "a condition in which all functions of the body and mind are normally active", and (2) "a state of complete physical, mental, or social well-being and not merely the absence of disease or infirmity", which is the World Health Organization's definition of health developed in 1948 that considers various levels of health. According to the Urimalsaem (an innovative open, collaborative dictionary) of the National Institute of the Korean Language [ 16], "quality of life" means "the degree of value, meaning, and satisfaction gained from living", and the Cambridge Dictionary [ 17] defines it as "the level of satisfaction and comfort that a person or group enjoys". Combining the above dictionary meanings, HRQOL can be defined as the degree of value, meaning, and satisfaction that individuals or groups perceive in various dimensions of life related to health.
2) Comparison with similar concepts
Health status and quality of life, which are similar concepts to HRQOL, were analyzed to clarify this potentially ambiguous concept by examining the similarities and differences between concepts.
Health status refers to an abnormal condition considering biological dysfunctions or symptoms. It also includes an assessment of morbidity, mortality, impairment, and anthropometric measures (e.g., height, weight, and body mass index) of an individual or population [ 10, 18]. Contrarily, quality of life is a broader concept than health status, clinical symptoms, or functional disability, as it refers to "an individual's perception of their position in life in the context of the culture and value systems in which they live and in relation to their goals, expectations, standards, and concerns". It is a comprehensive concept that encompasses all the factors that affect an individual's life [ 19]. HRQOL is sometimes treated as a narrower concept than quality of life, which covers all aspects of life, such as health, citizen participation, governance, and work-life balance [ 19, 20]. In the context of chronic illness, HRQOL is sometimes used interchangeably with quality of life because health affects many aspects of life, either directly or indirectly [ 19, 21]. In other words, these patterns suggest that areas of life related to health can appear in various ways depending on the context and situation in which an individual is placed.
3) Uses of health-related quality of life in various academic fields
HRQOL has been examined in various academic fields whose scope encompasses human health and well-being, such as medicine, nursing, public health, and social welfare. Furthermore, HRQOL has been expressed in many different forms because the concept is highly abstract and complex.
From the perspective of health policy, HRQOL is the health value assigned to various health conditions, and is converted into quantified values such as quality-adjusted life-years (QALYs) to evaluate the efficacy of health programs [ 19]. Similarly, in clinical medicine, HRQOL has been recognized as an important outcome indicator in clinical research, especially in phase 3 clinical trials designed to evaluate the effectiveness of treatment, expanding the scope of medical treatment quality assessment [ 22]. On the one hand, in social welfare and disability studies, HRQOL focuses on how individuals' unique life experiences and values interact with various health domains beyond the functional perspective of objectively evaluating clinical conditions and confirming the degree of damage to life [ 23, 24]. In this context, Park [ 24] pointed out that the most important factor in the quality of life of people with epilepsy is the balance between an individual's expectations and their level of actual experiences. She claimed that it is important to subjectively evaluate the quality of life by considering individuals' unique situations beyond objective indicators, such as the number of seizures and side effects of drugs. On the other hand, medical anthropologists who have focused on the temporal dimension of HRQOL clearly distinguished between "disease", defined as a medical diagnosis, and "illness", defined as a process that changes at different stages of the disease and different points in an individual's life. They assessed HRQOL with a focus on the experience of illness [ 9]. Loiselle et al. [ 25] captured changes in HRQOL over time in children newly diagnosed with epilepsy. They identified the unique trajectory of HRQOL and its key predictors, including side effects, behavioral problems, and parental fear and concerns. A study by Loiselle et al. [ 25] focused on volatility over time and provided evidence that the ability to identify risk groups whose HRQOL continues to deteriorate over time has significant implications for future intervention provisions. According to studies that attempted a context-focused approach to HRQOL, aspects of the environment including parents, families, peer groups, schools, and communities contribute to children's HRQOL and regulate the effects of disease and treatment on them [ 9]. Maia Filho Hde et al. [ 26] indicated that HRQOL in children with epilepsy is a multidimensional structure that deals with the perceptions of disease burden experienced by individuals in various aspects of life, such as disease characteristics, psychological consequences, social insertion, and educational achievement. Based on socio-ecological and system theory perspectives, Lach et al. [ 27] proposed an expanded conceptual model for HRQOL in youth with epilepsy. This model expanded the structure beyond the level of impairment (epilepsy and comorbidities) to child factors (psychosocial functioning), family processes, and community levels, which had not been considered as having potential mediating effects on HRQOL. They emphasized that HRQOL in children with epilepsy requires an exploration of each child's characteristics and context. Chon et al. [ 28] applied an ecological model to the HRQOL of local residents based on the view that human behavior is formed, changed, and maintained in the process of interacting with social, physical, and environmental factors belonging to or related to the individual, as well as the expression of individual perceptions and will. Through this, they identified that personal factors such as gender, subjective health status, perceived self-efficacy, perceived benefit or barrier, and microsystems expressed as social networks have a positive effect on HRQOL. Additionally, as the social and physical environment in the community, such as social overhead capital and medical facilities (constituting a mesosystem), was found to be the strongest factor associated with HRQOL, researchers suggested the need to expand opportunities for programs, education, and events based on high accessibility and convenience. Park and Baek [ 29] presented the HRQOL of children in three dimensions: intrapersonal, interpersonal, and organizational factors. They emphasized that the impact of interpersonal and organizational factors, such as family structure, peer support, and the use of community support centers, as well as intrapersonal factors, such as health perceptions and healthpromoting behaviors, should not be overlooked in understanding children's HRQOL. Boling et al. [ 30], who focused on the social stigma of children with epilepsy and their life experiences, reported that misunderstandings about diseases and psychosocial problems caused by them may have a greater impact on the quality of life of children with epilepsy than clinical factors, such as drug side effects. In other words, misconceptions or prejudices about epilepsy lead to negative attitudes and atmospheres in society, and children with epilepsy experience various types of discrimination in life, which in turn can lead to low self-esteem, restrictions on the formation of social relationships and activities, and social isolation [ 30]. Accordingly, Park [ 24] suggested that, as the purpose of epilepsy treatment is not only to control seizures but also to improve the quality of life, it is necessary to support social benefits, including the activation of a support system for people with epilepsy. In addition, she suggested that ongoing education and publicity to correct superstitions or prejudices about people with epilepsy could lead to changes in awareness and improve the quality of life for people with epilepsy. Furthermore, paying attention to the economic effect of community resources on improving the HRQOL of children with epilepsy, Pal et al. [ 31] reported that innovative interventions using existing community resources are cost-effective ways of improving HRQOL and psychosocial outcomes in children with epilepsy.
2. Determining the Defining Attributes
Defining attributes are those "characteristics of concepts that appear repeatedly". The defining attributes of HRQOL in children with epilepsy that repeatedly appear in the literature are as follows: health status, inner strength, close relationships, a resource-rich community, social acceptance, and changeability.
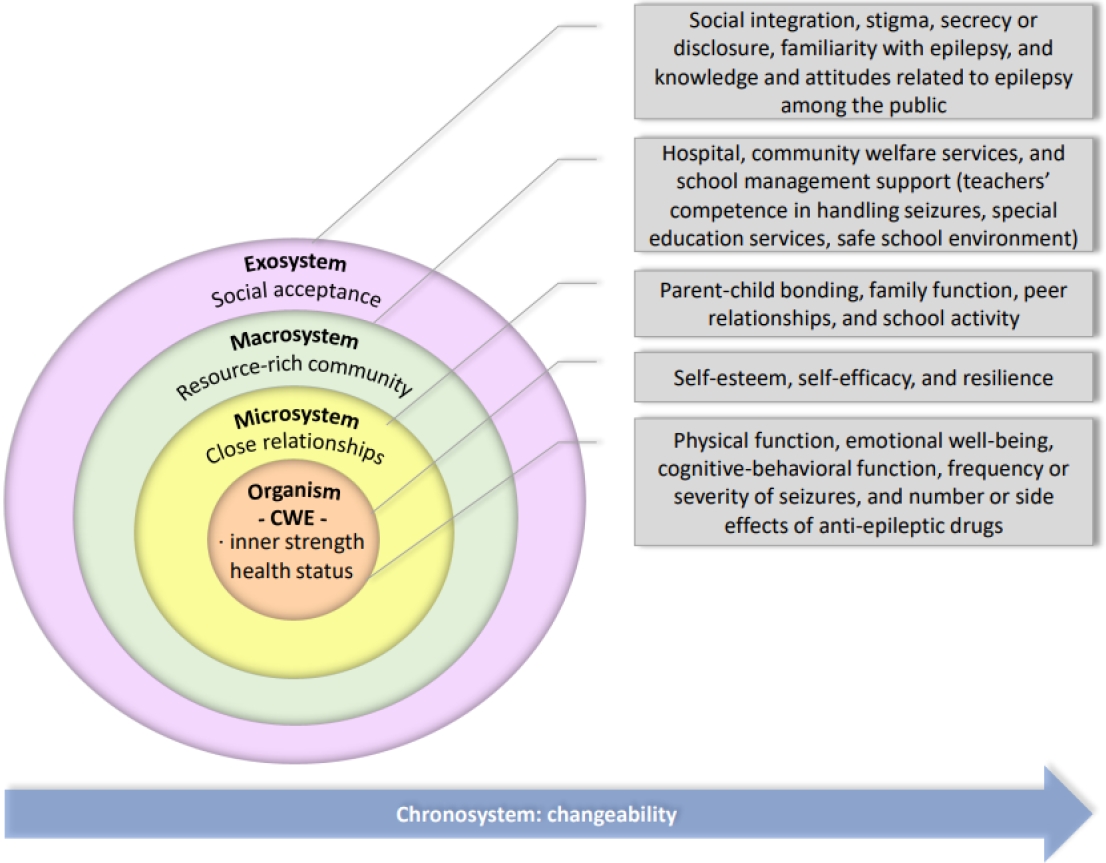
Concept analysis is a strategy used to examine the semantic structures of concepts. In this study, the ecological paradigm was maintained for structuring the concept of HRQOL in children with epilepsy because the defining attributes enabled a broad approach to the relationship between children with epilepsy and the environment ( Figure 2).
1) Organism: intrapersonal factors of children with epilepsy (health status, inner strength)
Health status, including clinical aspects such as the frequency or severity of seizures and number or side effects of medications, has a primary effect on HRQOL in children with epilepsy. Here, health status includes physical and mental health, as well as cognitive and behavioral functions that show problems, because diseases cause difficulties in an individual's daily life or role performance. In addition, individuals' unique inner resources such as self-esteem and self-efficacy are strongly related to HRQOL in children with epilepsy, and their presence plays an important buffer in attenuating the negative effects of factors that deteriorate HRQOL [ 3, 25, 32- 39].
2) Microsystem: relationships with important others or tightknit groups (close relationships)
According to Bronfenbrenner's [ 40] ecological system theory, the microsystem, which is the child's most immediate environment, can directly affect children's growth and development. Bronfenbrenner emphasized that the microsystem is a very important context, especially in infancy and childhood. A literature review showed that experiences in interactions and relationships with significant others or belonging groups, such as parents, family, friends, and schools, positively or negatively affected HRQOL in children with epilepsy [ 32, 34, 36- 38, 41, 42].
3) Macrosystem: abundance of community resources that children with epilepsy do not actively participate in, but indirectly affect their health-related quality of life (resource-rich community)
It was found that the HRQOL of children with epilepsy should be considered beyond the microsystem directly related to the child. Community resources, such as healthcare facilities for disease management, psychosocial interventions, epilepsy-related education, school personnel trained to deal with and handle seizure attacks, and facilities free of physical damage, have been used as external systems to improve HRQOL in children with epilepsy [ 5, 32, 35, 41, 43- 50].
4) Exosystem: sociocultural value systems that embrace children with epilepsy (social acceptance)
Cultural differences exhibit specific patterns in the level of quality of life [ 51], and an exosystem composed of a broad value system such as beliefs, norms, and identities underlying a particular culture influences children's experiences [ 40]. When people with epilepsy feel accepted in society, they make efforts to integrate epilepsy into their lives and display a more positive attitude toward life [ 52]. However, social stigma against a certain group can make them unable to accept themselves, putting their behaviors under the control of society [ 53]. In particular, social stigma experienced in childhood, when self-identity is not fully established, can act as a risk factor for children with epilepsy to form a negative self-concept and perceive life as unhappy [ 30, 35, 37, 42, 51, 54- 56].
5) Chronosystem: change can occur according to the configuration of perceptions about the significant events and environment of children with epilepsy, which dynamically change throughout the lifespan (changeability)
HRQOL in children with epilepsy was found to be dynamically changeable depending on the configuration of perceptions of events with a significant impact on health throughout life, such as the course of illness, developmental stage, and medical events (e.g., seizures, medication changes, or surgery) [ 25, 36- 38, 45, 57- 61].
3. Constructed Cases
1) Model case
A model case contains all the defining attributes of a concept, and it is an example that accurately represents the concept.
A was diagnosed with epilepsy at the age of 9 years and has been taking medication for 3 years. He has remained seizurefree with no medication side effects, and his cognitive and behavioral functions are also developing normally without any specific problems (health status). Although A sometimes lags in academic activities due to epilepsy, he firmly believes that he will be able to do just as well as his other friends if he takes his medications regularly and takes care of himself according to his doctor's instructions (inner strength). A's friends do not make fun of or ignore his illness, but rather visit A's house and stay with him so that A, who has limited outdoor activities, does not feel bored or lonely (close relationships).
In the early days when he was diagnosed with epilepsy, he had to take many medications every day. As a result, he always had no energy, suffered from drowsiness, and had difficulties in his daily life because of unexpected seizures. Subsequently, while on the ketogenic diet, he regained vitality and was able to return to his daily life (changeability). When A was diagnosed with epilepsy, his school conducted campaign activities in cooperation with the public health center with the goal of preventing safety accidents, supporting health care, and improving awareness of students with epilepsy. Consequently, safety devices were established after re-examining the safety management of the school facilities, and teachers gained the professional competence to efficiently respond to his seizures and perform first aid (resource-rich community). In addition, nearby residents became willing to accept their neighbor A with epilepsy and moved away from negative perceptions such as hateful looks, misunderstandings, and prejudices against epilepsy or seizures (social acceptance).
2) Borderline case
A borderline case contains some of the defining attributes, but not all of them; therefore, it cannot be regarded as representative of the concept.
B was diagnosed with epilepsy a year ago, and now her symptoms are not severe, so she is living a normal life and maintaining health and function like other people her age (health status). B considers herself valuable and precious, and she always promises that she will not give up and that she will persevere even if her epilepsy worsens and interferes with her life (inner strength). B believes that this is because she has family and friends who always support her and are present by her side as a driving force to keep a positive mindset even in an unstable future because of epilepsy (close relationships).
3) Related case
A related case is an example that relates to a concept but does not include the defining attributes—that is, one that superficially resembles the target concept but contains a different meaning when examined in detail.
C was diagnosed with epilepsy at the age of 5 years due to the neurological sequelae of encephalitis. C is currently homeschooled because of long-term inpatient treatment, and she is short compared to her age and has gained weight slowly. Ever since she was diagnosed with epilepsy, the whole family's attention has been focused on her, and everything revolves around her. C's mother quit her job to take care of C, and she thinks that it is her fault that C is sick, so she does everything her daughter wants.
4) Contrary case
A contrary case is described as an explicit example that is clearly unrelated to the concept.
D was diagnosed with epilepsy in the fifth grade of elementary school. She is currently on medication and is taking valproic acid and levetiracetam for treatment (absence of health status). The hospital in the area where D lives does not have a pediatric neurology center, so she has to miss school or leave early to receive medical treatment (absence of a resource-rich community). Because of this, she is often unable to attend various school activities, is often bullied because of the lack of opportunities to spend time with friends, and does not adapt well to school life (absence of close relationships). In the early stage of epilepsy, D had a seizure at the neighborhood playground. Subsequently, when she walked around the neighborhood, her neighbors consciously distanced themselves from her and feared her. In addition, her application to register at a physical education academy was rejected because she had epilepsy (absence of social acceptance). She feels useless and frustrated, thinking that her misfortune will not improve even though she is controlling her symptoms well without seizures after epilepsy surgery (absence of inner strength and changeability).
4. Antecedents and Consequences
Antecedents are events or conditions that occur before a concept is created. As a result of the literature review, the antecedents of HRQOL in children with epilepsy were identified as having epilepsy and interactions with the multidimensional ecological systems that are directly or indirectly related to children with epilepsy. Along with the medical diagnosis of epilepsy, children develop a different identity—a life coexisting with epilepsy. In this long journey, dynamic interactions with the ecological systems that are directly or indirectly related to the health and life of children with epilepsy lead to the formation of perceptions about HRQOL in children with epilepsy [ 3, 26, 27, 32, 37, 62]. In turn, the formation of perceptions of HRQOL in children with epilepsy results in positive or negative emotional experiences related to their health and lives. In other words, children with epilepsy form subjective perceptions of their health and life in their relationships with the multidimensional ecosystem. Consequently, children with epilepsy experience positive emotions such as satisfaction, happiness, hopefulness, and stability or negative emotions such as dissatisfaction, unhappiness, frustration, sadness, embarrassment, and self-pity [ 34, 41, 59, 60, 62, 63].
5. Empirical Referents
Empirical referents are types or categories of actual phenomena, and their existence makes it possible to prove the occurrence of the concept. Early measurement scales developed to measure HRQOL in children with epilepsy mainly focused on problems related to the function or dysfunction of children with epilepsy from a clinician's point of view and were used to assess and evaluate changes in the application of various treatments [ 5]. Ronen et al. [ 50] identified the attributes of HRQOL in children with epilepsy from the perspectives of both the children and their parents. Based on their attributes, Ronen et al. [ 50] developed the Health-Related Quality of Life Measure for Children with Epilepsy (CHEQOL-25), which comprises "interpersonal and social consequences", "worries and concerns", "intrapersonal and emotional issues", "secrecy", and "normality", and it can be inferred that these measurements considered both interpersonal and intrapersonal factors in children with epilepsy. CHEQOL-25 partially includes the attributes of the organism, microsystem, and macrosystem levels of HRQOL in children with epilepsy identified in this study but does not include the attributes of the exosystem level, a broader context that affects the health and life of children with epilepsy. By organizing the use cases of the concepts and measurements used in previous studies, we generated the following list of the empirical referents that can be used to recognize and measure the defining attributes of HRQOL in children with epilepsy:
• Health status: physical function, emotional well-being, cognitive-behavioral function, frequency or severity of seizures, and number or side effects of anti-epileptic drugs (AEDs) • Inner strength: self-esteem, self-efficacy, and resilience • Close relationships: parent-child bonding, family function, peer relationships, and school activity • Resource-rich community: hospital, community welfare services, and school management support (teachers' competence in handling seizures, special education services, safe school environment) • Social acceptance: social integration, stigma, secrecy or disclosure, familiarity with epilepsy, and knowledge and attitudes related to epilepsy among the public • Changeability: the trajectory of epilepsy, developmental stage, and transition
DISCUSSION
HRQOL is a concept frequently used in the medical and healthcare fields [ 10], and owing to the nature of this highly abstract and broad concept, it is likely to be interpreted without clear agreement or understanding apart from its frequency of use [ 22, 57]. In addition, even if some degree of agreement is reached regarding the concept of HRQOL, caution is necessary when assuming that the concept is used consistently because the critical attributes of the concept may differ among specific contexts and situations [ 6, 60]. Accordingly, this study was conducted to help clarify the concept by analyzing HRQOL in children who share the disease process of epilepsy according to the conceptual analysis method suggested by Walker and Avant [ 11]. The first attribute of the organism level is "health status", which is similar to three of the five major components (biological function, symptoms, and functional status) of the HRQOL model proposed by Ferrans et al. [ 21] in nursing. In addition, it is consistent with the view of the disablement model, which emphasizes HRQOL as an important value of healthcare outcomes, considers various health dimensions, and ensures that functional limitations and disabilities important to the patient are not overlooked [ 23]. Furthermore, HRQOL in children with epilepsy has historically evolved to include aspects of burden and impact of disease, complementing approaches limited to clinical aspects such as seizure frequency, severity, and side effects of AEDs [ 50]. In other words, the meaning of health status attributes has expanded with the evolution of the concept of HRQOL. From this point of view, when nursing research related to HRQOL in children with epilepsy should be informed by a full understanding of the specific and multifaceted influence of epilepsy on the child's health status, which will ultimately enable an appropriate and effective intervention. The second attribute of the organism level is "inner strength", which is an internal resource that enables children with epilepsy to adapt, change, and recover from adversities in life. Inner strength is difficult to realize through the cognitive approach of self-assessment alone and can be distinguished from "subjectivity", another unique attribute of individuals for which there is some consensus as an attribute of HRQOL. Similarly, inner strength was observed in the HRQOL of children with other chronic illnesses [ 64]. This is because they share long-term experiences of living with diseases regardless of the type of health problem, and in this process, an individual's unique inner resources act as a powerful factor in overcoming crises and increasing their overall satisfaction with their health and life. Therefore, nursing providers should recognize that global self-worth and reflection thereupon can lead to changes in the HRQOL of children with epilepsy, and consider including activities to develop and strengthen inner strength when providing nursing interventions to improve the HRQOL of children with epilepsy. Among the attributes of HRQOL in children with epilepsy identified in this study, "close relationships", "resource-rich community", and "social acceptance" could be interpreted and structured at an environmental level beyond the personal level. This aligns with the viewpoint of Drotar [ 9], who identified unmet needs for the evaluation of HRQOL in children and adolescents with chronic diseases and suggested implications for research and practice. Drotar [ 9] stressed that children and adolescents lack the ability or choice to change a given situation compared to adults; therefore, HRQOL in children and adolescents with chronic health conditions should include the characteristics of their situational and contextual factors. As a result of identifying empirical referents for the concept of HRQOL in children with epilepsy in this study, the existing measurements partially included environmental-level attributes derived in this study but were scattered across several domains, and the boundaries of meaning were ambiguous or unclear. In addition, none included the attribute of a "resourcerich community" [ 33]. Abundant community resources also lead to respect for and realization of the rights of children with epilepsy. Therefore, quantitative and qualitative reviews of community resources, including the expectations and needs of children with epilepsy for help or resource provision from the community, need to be considered as important attributes in explaining HRQOL. Based on the above results, HRQOL in children with epilepsy should be interpreted from a macro-holistic perspective. In other words, improving HRQOL requires multidisciplinary collaboration, not limited to the medical centers directly engaging in children's health care, but also among schools, communities, and governmental structures responsible for contributing to children's health and wellbeing. In the ecological system model, the chronosystem pursues dynamic and continuous changes through the reselection and reconstruction of children's environments and experiences [ 40]. Similarly, the attribute of "changeability" identified in this study was in line with the "dynamic" attribute frequently derived from previous studies on HRQOL, and provided the insight of temporal dimension into HRQOL in children with epilepsy [ 6, 25, 60]. This means that the construction of the perception of HRQOL in children with epilepsy during the disease process is not made independently but can be continuously changed while exchanging influences with various dimensions. In addition, the empirical referents of changeability emphasized the sensitivity or responsiveness to change occurring, and regarded them as important factors in discovering the therapeutic effectiveness and severity of disease in children with epilepsy [ 6, 57, 62]. This suggests that researchers should carefully consider the adjustment to the attribute of changeability in selecting measurement scales to evaluate and interpret the HRQOL in children with epilepsy. This study is meaningful because the concept of HRQOL, which has been used without a clear meaning in the absence of a rich understanding of its comprehensiveness and implications, was identified through an analysis considering the overall context of children experiencing epilepsy, which is a unique disease process. However, although Walker and Avant's [ 11] method of concept analysis has been recognized as very appropriate as a strategy for clarifying the meaning of existing concepts, there are some limitations as the concept analysis process is restricted to theoretical work and lacks an in-depth analysis of actual cases in the nursing field. Therefore, we suggest additional research on whether the attributes of the concept derived from this study reflect the real world. Furthermore, based on the results of this study, it is necessary to design and implement interventions using a multidisciplinary approach to improve HRQOL in children with epilepsy, and to develop measurements to accurately evaluate and validate their effects.
CONCLUSION
This study attempted to interpret the concept of HRQOL, which has been actively used in various academic fields without a sufficient understanding of the context and situation, from the perspective of children with epilepsy, using the concept analysis method of Walker and Avant [ 11]. Six attributes of HRQOL in children with epilepsy (health status, inner strength, close relationships, resource-rich community, social acceptance, and changeability) were identified in this study. These attributes are structured into five systems (organism, microsystem, macrosystem, exosystem, and chronosystem) that integrate the relationships between the attributes from an integrated and holistic perspective. The results of this study will help to understand the concept of HRQOL in children with epilepsy, support effective communication in practice settings that contribute to improving the health and well-being of children with epilepsy, and contribute to the development and expansion of interventions to improve their HRQOL.
REFERENCES
2. Aaberg KM, Gunnes N, Bakken IJ, Lund Søraas C, Berntsen A, Magnus P, et al. Incidence and prevalence of childhood epilepsy: a nationwide cohort study. Pediatrics. 2017;139(5):e20163908. https://doi.org/10.1542/peds.2016-3908
  3. Stevanovic D, Tadic I, Novakovic T. Health-related quality of life in children and adolescents with epilepsy: a systematic review In: Gadze ZP, editors. Epilepsy in children: clinical and social aspects. London: IntechOpen; 2011.
4. Park YS, Jeong EN, Yang JH. Lived experiences of life world for adolescents with epilepsy. Journal of Korean Academy of Fundamentals of Nursing. 2011;18(1):6-18.
6. Lee SY, Choi SC, Nah YH. Review: review on health-related quality of life (HRQL). Korean Journal of Neurogastroenterology and Motility. 2001;7(1):6-17.
8. Ko S. Calculation of healthy life expectancy in South Korea. Health Welfare Issue & Focus. 2014;(247):1-8.
9. Drotar D. Measuring health-related quality of life in children and adolescents: implications for research and practice. Mahwah (NJ): Lawrence Erlbaum Associates; 1998.
10. Yu SY. Measurement and variation of HRQoL: comparison among methods and utility score changes by health status [dissertation]. Seoul: Seoul National University; 2016.
11. Walker LO, Avant KC. Strategies for theory construction in nursing. 4th ed. Upper Saddle River (NJ): Pearson/Prentice Hall; 2005.
12. Tricco AC, Lillie E, Zarin W, O'Brien KK, Colquhoun H, Levac D, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Annals of Internal Medicine. 2018;169(7):467-473. https://doi.org/10.7326/M18-0850
  18. World Health Organization (WHO). Health status [Internet]. Houston (TX): International Association for Hospice & Palliative Care; 2009 [cited 2022 October 3]. Available from: https://pallipedia.org/health-status
20. Hand C. Measuring health-related quality of life in adults with chronic conditions in primary care settings: critical review of concepts and 3 tools. Canadian Family Physician. 2016;62(7):e375-e383.  22. Calvert MJ, Freemantle N. Use of health-related quality of life in prescribing research. Part 1: why evaluate health-related quality of life? Journal of Clinical Pharmacy and Therapeutics. 2003;28(6):513-521. https://doi.org/10.1046/j.0269-4727.2003.00521.x
  26. Maia Filho Hde S, Gomes Mda M, Fontenelle LM. Development and validation of a health related quality of life questionnaire for Brazilian children with epilepsy: preliminary findings. Arquivos de Neuro-Psiquiatria. 2005;63(2B):389-394. https://doi.org/10.1590/s0004-282x2005000300004
  27. Lach LM, Ronen GM, Rosenbaum PL, Cunningham C, Boyle MH, Bowman S, et al. Health-related quality of life in youth with epilepsy: theoretical model for clinicians and researchers. Part I: the role of epilepsy and co-morbidity. Quality of Life Research. 2006;15(7):1161-1171. https://doi.org/10.1007/s11136-006-0051-7
  28. Chon MY, Kang SY, Kim MY. Influencing factors of health-related quality of life in an local residents': based on ecological model. Journal of The Korean Society of Living Environmental System. 2021;28(1):39-48. https://doi.org/10.21086/ksles.2021.2.28.1.39
 29. Park J, Baek S. Ecological predictors of health-related quality of life (HRQoL) among children from low-income families in South Korea. Children and Youth Services Review. 2017;81:238-245. https://doi.org/10.1016/j.childyouth.2017.07.027
 32. Chew J, Carpenter J, Haase AM. Living with epilepsy in adolescence-a qualitative study of young people's experiences in Singapore: peer socialization, autonomy, and self-esteem. Child: Care, Health and Development. 2019;45(2):241-250. https://doi.org/10.1111/cch.12648
  33. Crudgington H, Collingwood A, Bray L, Lyle S, Martin R, Gringras P, et al. Mapping epilepsy-specific patient-reported outcome measures for children to a proposed core outcome set for childhood epilepsy. Epilepsy & Behavior. 2020;112:107372. https://doi.org/10.1016/j.yebeh.2020.107372
 34. Elliott IM, Lach L, Smith ML. I just want to be normal: a qualitative study exploring how children and adolescents view the impact of intractable epilepsy on their quality of life. Epilepsy & Behavior. 2005;7(4):664-678. https://doi.org/10.1016/j.yebeh.2005.07.004
 35. Kerr C, Nixon A, Angalakuditi M. The impact of epilepsy on children and adult patients' lives: development of a conceptual model from qualitative literature. Seizure. 2011;20(10):764-774. https://doi.org/10.1016/j.seizure.2011.07.007
  36. McEwan MJ, Espie CA, Metcalfe J, Brodie MJ, Wilson MT. Quality of life and psychosocial development in adolescents with epilepsy: a qualitative investigation using focus group methods. Seizure. 2004;13(1):15-31. https://doi.org/10.1016/s1059-1311(03)00080-3
  37. Ronen GM, Rosenbaum P, Law M, Streiner DL. Health-related quality of life in childhood disorders: a modified focus group technique to involve children. Quality of Life Research. 2001;10(1):71-79. https://doi.org/10.1023/a:1016659917227
  38. Thomson L, Fayed N, Sedarous F, Ronen GM. Life quality and health in adolescents and emerging adults with epilepsy during the years of transition: a scoping review. Developmental Medicine and Child Neurology. 2014;56(5):421-433. https://doi.org/10.1111/dmcn.12335
  39. Aronu AE, Uwaezuoke N, Chinawa JM, Bisi-Onyemaechi A, Ojinnaka NC. Health-related quality of life in children and adolescents with epilepsy in Enugu: need for targeted intervention. Nigerian Journal of Clinical Practice. 2021;24(4):517-524.  40. Bronfenbrenner U. Ecological systems theory In: Vasta R, editors. Six theories of child development: revised formulations and current issues. London: Jessica Kingsley; 1992. p. 187-249.
41. Hightower S, Carmon M, Minick P. A qualitative descriptive study of the lived experiences of school-aged children with epilepsy. Journal of Pediatric Health Care. 2002;16(3):131-137. https://doi.org/10.1067/mph.2002.119599
  43. Abdel Ghaffar NF, Asiri RN, Al-Eitan LN, Alamri RS, Alshyarba RM, Alrefeidi FA, et al. Improving public stigma, sociocultural beliefs, and social identity for people with epilepsy in the Aseer region of Saudi Arabia. Epilepsy & Behavior Reports. 2021;16:100442. https://doi.org/10.1016/j.ebr.2021.100442
 44. Bishop M, Boag EM. Teachers' knowledge about epilepsy and attitudes toward students with epilepsy: results of a national survey. Epilepsy & Behavior. 2006;8(2):397-405. https://doi.org/10.1016/j.yebeh.2005.11.008
 45. Ferro MA, Camfield CS, Levin SD, Smith ML, Wiebe S, Zou G, et al. Trajectories of health-related quality of life in children with epilepsy: a cohort study. Epilepsia. 2013;54(11):1889-1897. https://doi.org/10.1111/epi.12388
  46. Jantzen S, Muller-Godeffroy E, Hallfahrt-Krisl T, Aksu F, Pust B, Kohl B, et al. FLIP&FLAP-a training programme for children and adolescents with epilepsy, and their parents. Seizure. 2009;18(7):478-486. https://doi.org/10.1016/j.seizure.2009.04.007
  50. Ronen GM, Streiner DL, Rosenbaum P, Canadian Pediatric Epilepsy Network. Health-related quality of life in children with epilepsy: development and validation of self-report and parent proxy measures. Epilepsia. 2003;44(4):598-612. https://doi.org/10.1046/j.1528-1157.2003.46302.x
  54. Asnakew S, Legas G, Belete A, Tadele Admasu F, Demilie K, Alebachew Bayih W, et al. Knowledge and attitude of the community towards epilepsy in Northwest Ethiopia: a huge gap on knowledge and attitude of the community. Epilepsy & Behavior Reports. 2020;15:100422. https://doi.org/10.1016/j.ebr.2020.100422
 55. Austin JK, MacLeod J, Dunn DW, Shen J, Perkins SM. Measuring stigma in children with epilepsy and their parents: instrument development and testing. Epilepsy & Behavior. 2004;5(4):472-482. https://doi.org/10.1016/j.yebeh.2004.04.008
 56. Funderburk JA, McCormick BP, Austin JK. Does attitude toward epilepsy mediate the relationship between perceived stigma and mental health outcomes in children with epilepsy? Epilepsy & Behavior. 2007;11(1):71-76. https://doi.org/10.1016/j.yebeh.2007.04.006
 57. De Civita M, Regier D, Alamgir AH, Anis AH, Fitzgerald MJ, Marra CA. Evaluating health-related quality-of-life studies in paediatric populations: some conceptual, methodological and developmental considerations and recent applications. Pharmacoeconomics. 2005;23(7):659-685. https://doi.org/10.2165/00019053-200523070-00003
  58. Jain P, Smith ML, Speechley K, Ferro M, Connolly M, Ramachandrannair R, et al. Seizure freedom improves health-related quality of life after epilepsy surgery in children. Developmental Medicine & Child Neurology. 2020;62(5):600-608. https://doi.org/10.1111/dmcn.14390
 59. Schraegle WA, Titus JB. The relationship of seizure focus with depression, anxiety, and health-related quality of life in children and adolescents with epilepsy. Epilepsy & Behavior. 2017;68:115-122. https://doi.org/10.1016/j.yebeh.2016.12.009
 61. van Empelen R, Jennekens-Schinkel A, van Rijen PC, Helders PJ, van Nieuwenhuizen O. Health-related quality of life and self-perceived competence of children assessed before and up to two years after epilepsy surgery. Epilepsia. 2005;46(2):258-271. https://doi.org/10.1111/j.0013-9580.2005.27304.x
  62. Moffat C, Dorris L, Connor L, Espie CA. The impact of childhood epilepsy on quality of life: a qualitative investigation using focus group methods to obtain children's perspectives on living with epilepsy. Epilepsy & Behavior. 2009;14(1):179-189. https://doi.org/10.1016/j.yebeh.2008.09.025
 63. Chew J, Carpenter J, Haase AM. Young people's experiences of epilepsy: a scoping review of qualitative studies. Health & Social Work. 2017;42(3):167-176. https://doi.org/10.1093/hsw/hlx020
 64. Kim M. Health-related quality of life in adolescents with chronic diseases [dissertation]. Seoul: Chung-Ang University; 2018.
Figure 1.
Flow diagram for the selection of studies on health-related quality of life in children with epilepsy. 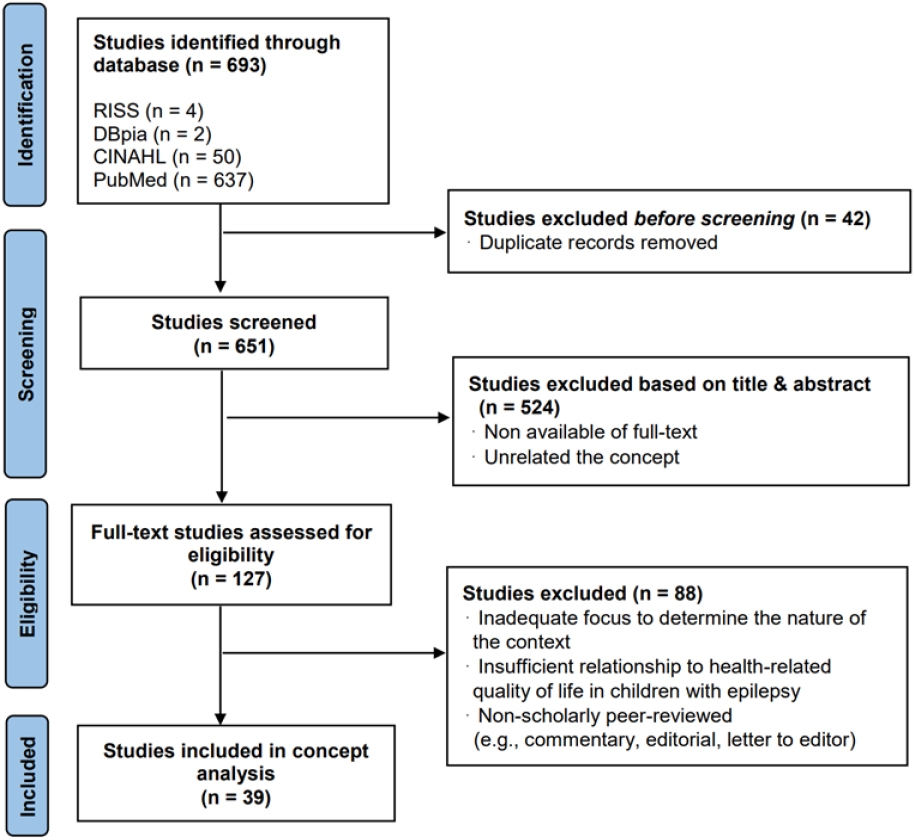
Figure 2.
Organization of the concept of health-related quality of life in children with epilepsy. CWE, children with epilepsy. 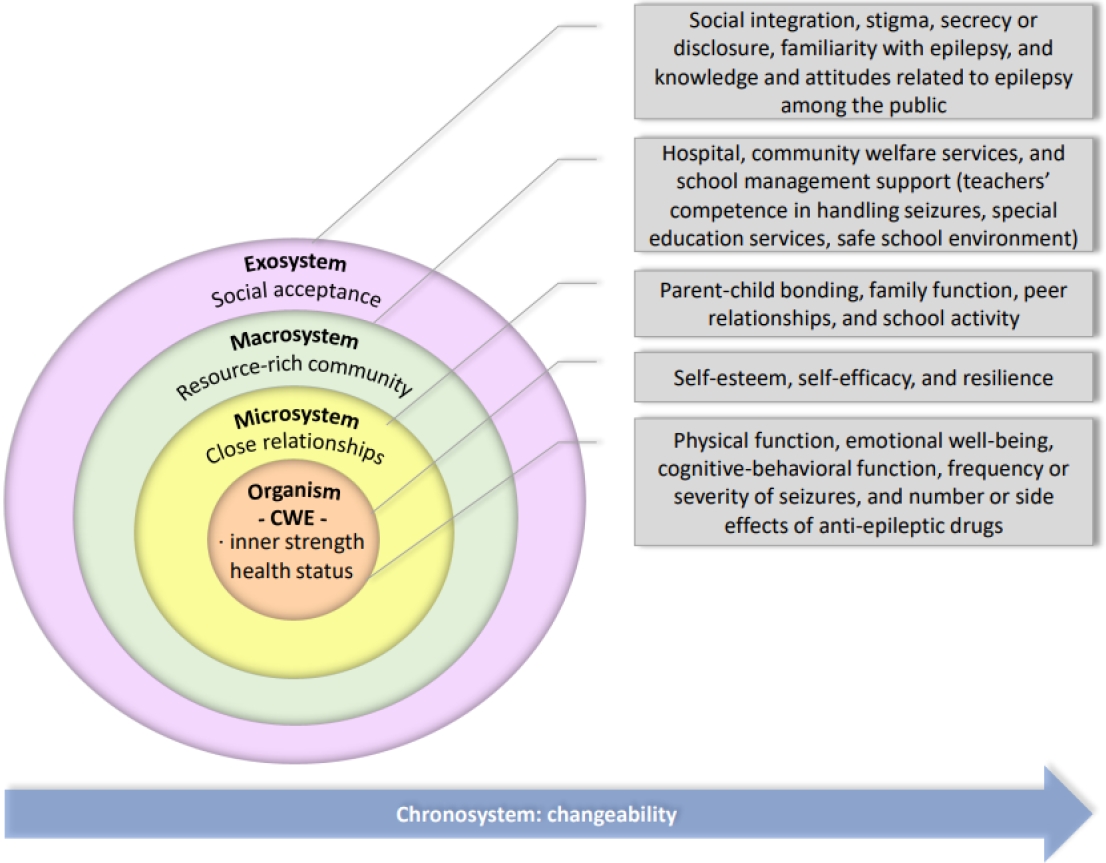
|
|