Factors associated with healthcare utilization for infant falls in South Korea: a cross-sectional online survey
Article information
Abstract
Purpose
Falls are a common cause of unintentional injuries in infants. This study was conducted to examine the patterns of healthcare utilization following infant falls in South Korea.
Methods
This cross-sectional descriptive study utilized an online survey designed to gather information regarding the general characteristics of parents and infants, fall-related variables, and healthcare use.
Results
The most serious falls identified by parents occurred at an average infant age of 6.97 months. Most fall incidents took place indoors (95.7%), and many occurred under the supervision of caregivers (68.0%). Following the fall, 36.4% of the participants used healthcare services. Logistic regression analysis revealed that healthcare use following an infant fall was significantly associated with being a firstborn child (odds ratio [OR]=5.32, 95% confidence interval [CI], 2.19-15.28) and falling from a caregiver's arms (OR=4.22; 95% CI, 1.45-13.68).
Conclusion
To prevent and decrease the frequency of infant falls, improvements are needed in both the domestic environment and parenting approaches.
INTRODUCTION
Falls represent one of the most common types of unintentional injury in infants, accounting for 50.8% of injuries in those under 12 months old [1]. These falls typically take place in the home, frequently involving infants falling off beds, sofas, strollers, or from a parent's arms onto the floor [2]. In contrast, falls in children between the ages of 1 and 5 years are more likely to occur on playgrounds, balconies, or during play with toys [3,4]. The mechanisms and characteristics of injuries from falls also vary according to age.
Infant falls can result in skull fractures, brain injuries, concussions, and skin damage [5]. Infants under 1-year-old are at an elevated risk of serious injuries from falls, including skull fractures or brain hemorrhages, compared to children aged 2 to 4 years [3,6]. Prior research has indicated that severe injuries tend to occur when infants younger than 3 months fall from a height exceeding 50 cm, most often from the arms of parents, down stairs, or onto the street [7].
When an infant experiences a fall at home, parents frequently face uncertainty about the appropriate course of action, particularly if symptoms are not immediately evident. The critical choice between seeking medical attention and monitoring the situation at home can be complex. Parents often turn to their peers or social media platforms for advice, underscoring the need for available information [8].
Previous studies of infant falls have primarily been concentrated on identifying the factors influencing injury severity among infants brought to the emergency department (ED) [3,7,9]. However, it is crucial to conduct a comprehensive evaluation of the characteristics of infant falls and the full spectrum of healthcare utilization. Based on the results, the severity of injuries and the appropriateness of medical use can be evaluated. However, research on infant falls in South Korea remains insufficient, with a dearth of data regarding the circumstances and manner of falls occurring within this population. Furthermore, given that some infants may not be brought to healthcare professionals after a fall, it is vital to examine personal and situational factors that could influence healthcare use in this situation. A thorough investigation that includes the specifics of fall incidents and subsequent healthcare utilization could offer essential insights for the development of safety education and the promotion of a safer home environment.
Therefore, this study was undertaken to examine the patterns of healthcare utilization following falls among infants in South Korea, with the following specific objectives: first, to investigate the mechanisms that underlie falls in infants under 12 months old; and second, to identify the factors influencing healthcare utilization.
METHODS
Ethics statement: This study was approved by the Public Institutional Bioethics Committee, designated by the Ministry of Health and Welfare (No. 2022-0727-002). Informed consent was obtained from all participants.
1. Study Design and Setting
This study employed a cross-sectional descriptive research design, utilizing an online questionnaire completed by parents of infants who had experienced falls. Data collection took place from July 16 to August 22, 2022 in South Korea. The study adhered to the reporting guidelines for online survey research [10].
2. Participants
Brief information regarding the study objectives, protection of data, and informed consent was posted in several online communities for parents. Potential participants who reached out to the authors for more details were screened using specific inclusion criteria. These criteria included being a primary caregiver (mother or father) of an infant who had experienced a fall prior to 12 months of age and was currently under 15 months old, being a guardian aged 18 years or older, and possessing the ability to read and understand Korean. The criterion of an infant age of 15 months or younger was used to minimize the potential for parental recall bias. Informed consent was obtained from those who voluntarily agreed to participate in the study. Following this, a hyperlink to the questionnaire was sent to the participants.
The rule of 10 events per variable has been deemed acceptable for determining the minimum necessary sample size for binary logistic regression models [11]. Our calculations indicated that a minimum of 208 participants would yield a power of 80% to detect an odds ratio (OR) of 1.5, assuming a probability of 0.5 and a 5% significance level. These calculations were performed using G*Power 3.1.9.4 (University of Dusseldorf). Considering a potential dropout rate of 10%, we aimed to recruit a total of 232 participants.
3. Variables and Measurements
Authors conducted a comprehensive review of the literature to investigate the risk factors, circumstances, and outcomes associated with infant fall incidents, with the aim of developing a questionnaire [3,7,12,13]. The preliminary version of the questionnaire was tested for face validity by three mothers of infants, after which it was revised. The final version of the questionnaire comprised 29 items and required approximately 5 to 10 minutes to complete. The questionnaire was designed to gather data on variables related to parents (age, sex, family members, education level, household, occupation, support for infant care, and experience with infant safety education), infants (age and birth order), and falls. The fall-related variables included data on the first infant fall, the total number of infant falls, the most serious fall as identified by the parents (including the age and developmental status of the infant, location, circumstances, and level of supervision), and healthcare utilization (type of healthcare services, medical examinations, and diagnosis). The primary outcome variable was the utilization of healthcare services (outpatient department [OPD] visit, ED visit, or hospital admission) following an infant fall. The questionnaire, which was validated in a pilot study, was administered online using Google Forms (https://docs.google.com/forms; Google).
4. Statistical Analysis
The data were summarized using descriptive methods. Categorical variables were represented by frequencies and percentages, while continuous variables were expressed as means and standard deviations. We assessed each variable for normality and used either the x2 test or the t-test to identify statistical differences. To determine the factors associated with healthcare use following infant falls, we fitted binary logistic regression models. We first conducted univariable logistic regression, then included variables that were relevant (p<.1) in a multivariable logistic regression model. The ORs and 95% confidence intervals (CIs) were also reported. The analysis was performed using R version 4.0.3 (R Foundation for Statistical Computing), with p-values less than .05 considered to indicate statistical significance.
RESULTS
Of 237 responses that were identified, 231 were incorporated into the final analysis. This was achieved after the exclusion of two duplicate responses, three responses from parents with infants older than 15 months, and one response from an individual whose infant had never experienced a fall.
1. Participant Demographic Characteristics
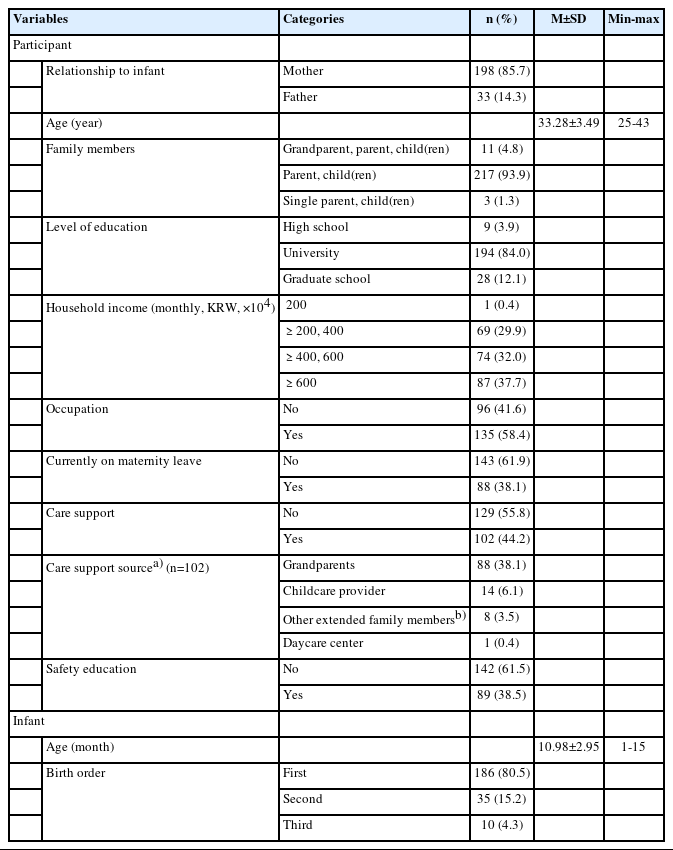
Most participants were mothers (85.7%), with a mean age of 33.28 years (standard deviation [SD]: 3.49 years), and most had completed higher education (university or higher) (Table 1). More than half of the parents (55.8%) reported not receiving any childcare support. The remaining participants indicated receiving support from various sources, including grandparents (38.1%), childcare providers (6.1%), and other extended family members (3.5%). Only 38.5% of the parents had received safety education on infant care. The infants in the study had a mean age of 10.98 months (SD: 2.95 months), and the majority were firstborns (80.5%).
2. Fall-related Characteristics
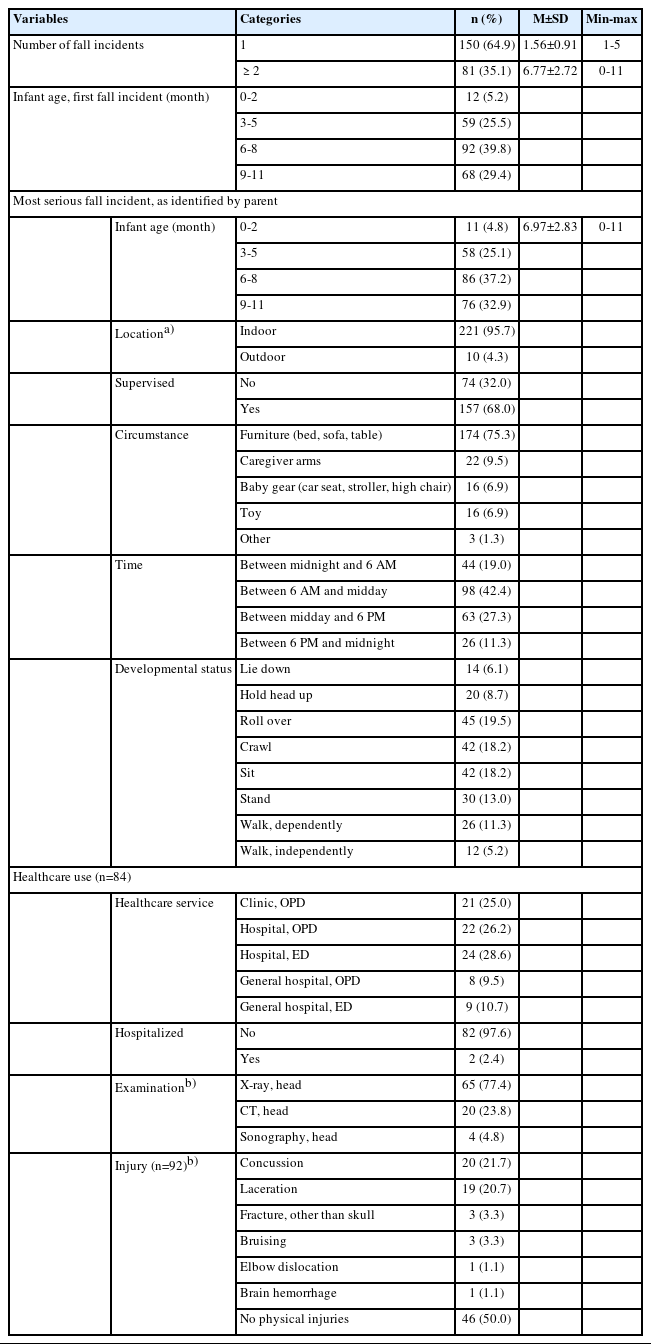
In this study, 35.1% of the infants had experienced multiple falls (Table 2). The average infant age at the time of the first and the most severe fall was 6.77 months (SD: 2.72 months) and 6.97 months (SD: 2.83 months), respectively. Of these most severe falls, 68.0% occurred under the supervision of a caregiver, and 95.7% took place indoors, predominantly within the infants' homes. The most common circumstance associated with an infant fall was furniture, representing 75.3% of incidents. This was followed by falls from the arms of a caregiver (9.5%), baby equipment (6.9%), and toys (6.9%). The majority of the most severe infant falls occurred between 6 AM and midday (42.4%), with the next most common period being midday to 6 PM (27.3%). A total of 34.3% of the falls occurred before the infant could crawl; this included those who could only lie down (6.1%), who could hold their heads up (8.7%), and who could roll over (19.5%).
Of the 84 participants (36.4%) who used healthcare services due to infant falls, 39.3% visited the ED. This percentage was further divided into 28.6% for hospital ED visits and 10.7% for general hospital ED visits. Only 2.4% of the infants required hospitalization. Among the infants who utilized healthcare services, 77.4% underwent a head X-ray scan, while 23.8% received a head computed tomography (CT) scan. Notably, most patients (50.0%) did not receive a diagnosis of a fall injury (50.0%). However, brain hemorrhage was reported in one infant (1.1%). The most common fall injury diagnosed in infants was concussion (21.7%), followed by laceration (20.7%).
3. Factors Associated with Healthcare Use
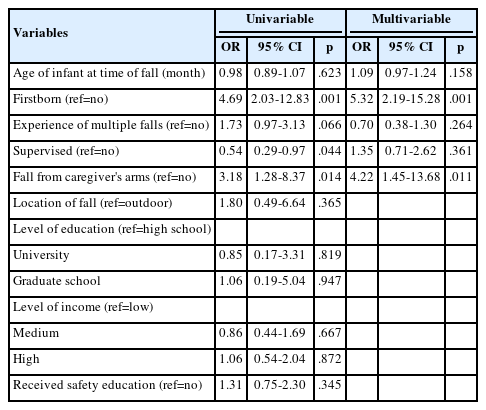
After the univariable regression analysis, the final model incorporated covariates such as the age of the infant at the time of the serious fall, whether the child was a firstborn, the occurrence of multiple falls, the level of supervision, and whether the fall happened from the arms of a caregiver. The category of "no" was used as the reference group (Table 3). The maximum variance inflation factor was 2.21, indicating the absence of multicollinearity in the model. The multivariable binary logistic regression model revealed significant associations between the use of healthcare following infant falls and two factors: being a firstborn child (OR=5.32; 95% CI, 2.19-15.28) and experiencing a fall from the arms of a caregiver (OR=4.22; 95% CI, 1.45-13.68). However, the age of the infant, the occurrence of multiple falls, and the level of supervision were not significantly associated with the use of healthcare services.
DISCUSSION
In this study, we explored characteristics of falls in infants under 12 months of age and subsequent healthcare utilization. The most frequent age range at which the first and most serious fall incidents occurred was 6 to 7 months. This finding is consistent with a previous study examining infants who visited the ED due to falls, which reported a median age of 7 to 8 months [7,9]. Given that infants typically start rolling over at 4 to 6 months of age, parents must exercise particular caution during this period. They may unintentionally cause a fall by placing the infant on a high surface, such as a bed or a sofa. Therefore, parents should prioritize preventive measures, such as refraining from leaving the baby unattended on high surfaces as soon as the infant begins to roll over.
Most falls occurred in indoor settings, although some incidents did take place outdoors, such as on playgrounds, streets, and the stairs of buildings. A study carried out in Spain that investigated infant visits to the ED similarly revealed that the majority of falls happened at home (83.5%) [7]. This could be due to infants primarily spending time indoors at home, a situation potentially exacerbated in the present investigation by the decrease in outdoor activities in the 2022 study period due to the ongoing coronavirus pandemic. Cultural factors may also play a role in the amount of time infants spend at home. As a result, future research must include a thorough analysis to clarify the reasons behind the high frequency of falls at home and to devise effective preventative strategies.
In this study, falls involving furniture such as beds, sofas, and tables were often observed during the morning hours, between 6 AM and noon. Consistent with previous research, household furniture or fixtures [12,14] and nursery equipment [7] were identified as common causes of falls in infants under 12 months. These findings imply that infants may be prone to falls during naps on beds or sofas, or while engaging in play on furniture. Notably, falls related to beds are the primary cause of fractures and traumatic brain injuries in infants [9]. Consequently, it is essential to ensure that infants sleep in cribs, rather than in their parents' beds, to prevent falls and associated injuries.
Among the study participants, instances of infant falls were reported in both the presence and the absence of supervision, with 55.8% of incidents occurring without caregiver support. These unsupervised falls may have transpired while caregivers were preoccupied with other tasks, a situation potentially compounded by the absence of assistance. However, infant falls can occur abruptly, even under parental supervision [7,14]. Given their rapid motor development, which includes turning over, sitting, and standing, infants necessitate increased parental vigilance. Therefore, it is imperative to enhance caregiver supervision and support. This can be achieved through measures such as making environmental adjustments, refraining from placing infants on elevated surfaces, and ensuring the proper use of baby products.
The results of this study indicate that infants who received medical attention after a fall primarily underwent diagnostic procedures such as radiography and CT scans. A study conducted in the United Kingdom revealed that 16.4% of infants under 12 months who visited the ED due to falls were administered CT scans [13]. A direct comparison of the frequency of CT scans between this study, which encompassed both EDs and OPDs, and the UK study is difficult due to the differing healthcare systems. Crucially, however, conducting CT scans on young children necessitates sedation and incurs higher costs than radiography, regardless of the healthcare system. Therefore, it is essential to evaluate the level of consciousness, the mechanism of injury, and the occurrence of seizures via a checklist when managing infant head injuries [15]. A CT scan should only be performed if it is deemed necessary based on this evaluation. Currently, no standardized guidelines are available in Korea for CT scans in children with head injuries, underscoring the pressing need for such guidelines to ensure uniform examination practices in both outpatient and emergency settings.
This study indicated that firstborn children were particularly likely to receive healthcare services following a fall. The psychological distress experienced by parents when their child is injured can be amplified for first-time parents, who may grapple with heightened anxiety and diminished coping ability due to their unfamiliarity with child-rearing. The findings of this study are consistent with prior research, which suggests a correlation between birth order and the frequency of ED visits and hospitalizations following infant vaccinations [16]. Furthermore, when infants fall while being held by a caregiver, the likelihood of subsequent healthcare utilization increases. Although these incidents occur less frequently than household falls, they contribute substantially to the overall number of infant falls [3] and are associated with abnormal findings on CT scans [13]. Infants may fall from their parents' arms due to a slip or if the parent falls asleep while holding them. In such instances, infants can fall from a height greater than that of a bed or sofa, potentially leading parents to perceive a heightened risk of injury and thus seek medical attention.
In the present study, factors such as the age of the infant, previous falls, and level of parental supervision demonstrated no significant correlation with the utilization of medical facilities. Furthermore, the infant's developmental stage and parental safety education did not display any significant influence on fall-related healthcare utilization in the univariate analysis and were therefore excluded from the final regression model. The regression analysis conducted in this study emphasizes that the decision to seek medical care following a fall is primarily driven by the parents' perception of the fall risk and the actual risk involved. Although this study included factors such as the timing, location, and mechanism of the fall, it did not consider the impact of the height of the fall and the surface on the severity of the injury. Consequently, additional research is required to evaluate the effect of these factors on the utilization of medical facilities. Moreover, since this study involved data gathered during the spring and summer, and considering the seasonal variations in the occurrence of falls [17], future research should incorporate seasonal factors.
Parental knowledge is associated with injury prevention behavior, yet the practical implementation of such preventative behavior frequently does not meet expectations [18]. Community nurses should provide parents with specific guidance on effective fall-prevention practices. They should also offer counseling and support to help parents manage falls and make informed decisions about seeking medical care. A potential limitation of this study is the reliance on self-reported parental data regarding infant fall incidents, which could lead to recall bias. To improve internal validity and credibility, future research should be designed to reduce the time gap between fall incidents and data collection. Furthermore, a prospective cohort study is suggested to identify factors influencing infant fall prevention.
CONCLUSION
This study provides valuable insight into infant falls in daily life, illuminating their mechanisms and related healthcare usage. These results can support community nurses in the creation and implementation of safety and fall prevention education for parents of infants. Furthermore, this research provides vital direction for nurses in acute care centers, emphasizing the relevant factors that should be evaluated in relation to infant falls.
Notes
Authors' contribution
Conceptualization: all authors; Data collection, Formal analysis: all authors; Writing-original draft: all authors; Writing-review and editing: all authors; Final approval of published version: all authors.
Conflict of interest
No existing or potential conflict of interest relevant to this article was reported.
Funding
This work was supported by a 2022 Bucheon University Research Grant.
Data availability
Please contact the corresponding author for data availability.
Acknowledgements
None.